Acne
vulgaris
Salient
features
·
Acne
vulgaris is a common disorder of the pilosebaceous unit.
·
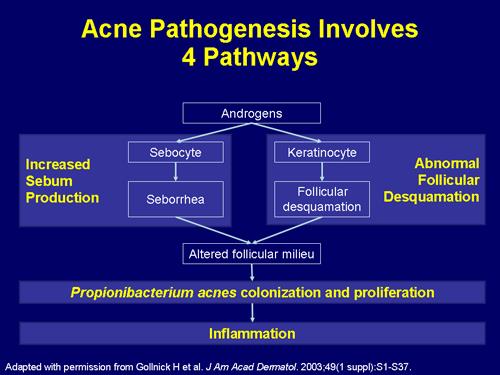
There
are four key elements of pathogenesis: (1) follicular epidermal
hyperproliferation, (2) sebum production, (3) the presence and activity
of Propionibacterium acnes, and (4) inflammation and immune
response.
·
Clinical
features include comedones, papules, pustules, and nodules on the face, chest,
and back.
·
Treatment
often includes combinations of oral and topical agents such as antimicrobials,
retinoids, and hormonal agents. Laser and light sources are additional
treatment options.
Introduction
Acne is a chronic
inflammatory disease of the pilosebaceous units.
It is characterized by the formation of open
and closed comedones, erythematous papules and pustules and in more severe
cases nodules, deep pustules and pseudocysts. Seborrhoea along with scarring
and post‐inflammatory erythema and/or
pigment changes is common features. While the course of acne may be
self-limiting, the sequelae can be life long, with pitted or hypertrophic scar
formation.
The central pathophysiological feature of
acne is increased androgenic stimulation and/or end-organ sensitivity of
pilosebaceous units leading to sebum hypersecretion and infundibular hyperkeratinization.
These events lead to Propionibacterium acnes proliferation and subsequent
inflammation.
There are two types of 5 alfa reductase, type
1 and type 2. Type 1 is most relevant in acne because sebaceous glands in acne
prone regions show abnormally high 5alfa reductase type 1 activity which
supports the end organ hyper-responsive to androgen theory for acne.
Epidemiology, including
Genetic and Dietary Factors
Acne is a common disorder affecting the majority of
adolescents and often extends into adulthood. Globally,
acne accounts for ~0.3% of the total and ~16% of the dermatologic disease
burden. Acne often heralds the onset of puberty. With a peak incidence
during adolescence, acne affects approximately 85% of young people between 12
and 24 years of age and is therefore a physiologic
occurrence in this group. With the general trend over the past few decades for
earlier puberty, preadolescent acne affecting children 7 to 11 years of age has
also become more common. While typically thought of as a disease of youth, acne
often continues to be problematic well into adulthood. In a survey-based study it
has shown that, 35% of women and 20% of men reported having acne in their 30s,
while 26% of women and 12% of men were still affected in their 40s.
The disease may be
minor, with only a few comedones or papules, or it may occur as the highly
inflammatory and diffusely scarring acne conglobata. The most severe forms of acne
occur more frequently in males, but the disease tends to be more persistent in
females, who may have periodic flare-ups before menstrual periods, which
continue until menopause.
Individuals
at increased risk for the development of acne include those with an XYY
karyotype or endocrine disorders such as polycystic ovarian syndrome,
hyperandrogenism, hypercortisolism, and precocious puberty. Patients with these
conditions tend to have more severe acne that is less responsive to standard
therapy.
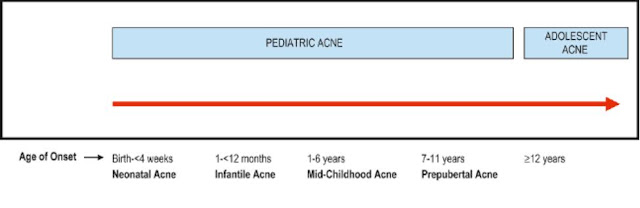
Pediatric acne is the
terminology applied to acne occurring from birth through 11 years of age; adolescent
acne describes patients from age 12 to adulthood.
Genetic Factors
The
precise role of genetic predisposition in the multifactorial pathogenesis of
acne remains to be determined. The number, size, and activity of sebaceous
glands is inherited. It is a widely belief that the tendency to have
substantial acne (including the nodular variant) runs in families, and an
association between moderate to severe acne and a family history of acne has
been observed in several studies.
Dietary Factors
The
relationship between diet and acne remains a subject of controversy. Several
observational studies in different ethnic groups have found that intake of
milk, especially skim milk, is positively associated with acne prevalence and
severity. Exacerbation of acne with the use of whey protein supplements for
body building has also been reported. In addition, prospective studies have
documented a link between a high glycemic-load diet and acne risk. A recent
investigation found that vitamin B12 supplementation
can potentially trigger the development of acne by altering the transcriptome
of skin microbiota, leading to increased production of proinflammatory porphyrins
by Propionibacterium acnes.
Pathogenesis
Factors
causing acne
The classical concept is that acne results from the
combination of increased sebaceous gland activity with hyperseborrhoea,
abnormal follicular differentiation with increased keratinization, microbial
hypercolonization of the follicular canal with P. acnes and increased
inflammation primarily through activation of the adaptive immune system. New
research results have led to a modification of this classical explanation as
more primary pathophysiological factors have been identified. Along with a
genetic predisposition, other major factors include androgens, pro‐inflammatory
lipids such as ligands of sebocyte peroxisome proliferator‐activated
receptors (PPAR) and other inflammatory pathways. In addition, neuroendocrine
regulatory mechanisms, diet and exogenous factors all may contribute to this
multifactorial process.
Inflammatory
cascades involved in acne pathogenesis.
The
development of acne involves the interplay of a variety of factors, including:
(1) follicular hyperkeratinization; (2) hormonal influences on sebum production
and composition; and (3) inflammation, in part mediated by P. acnes
Inflammatory
papule/pustule
·
Proliferation of P.
acne which up regulates innate immune response (e.g. via TLRs)
·
Mild perifollicular
inflammation (primarily neutrophils). Sebaceous lobule regression
Nodule
·
Marked perifollicular
inflammation (primarily T cells)
·
May lead to scarring
Follicular Hyperkeratinization
The microcomedo is thought to be the precursor of all
clinically apparent acne lesions. It forms in the upper portion of the follicle
within the lower portion of the infundibulum, the infrainfundibulum.
Corneocytes, which are normally shed into the lumen of the follicle and
extruded through the follicular ostium are retained
and accumulate due to increases in both follicular
keratinocyte proliferation and corneocyte cohesiveness, leading to the
development of a hyperkeratotic plug and a bottleneck phenomenon. The inciting
event for microcomedo formation is unknown, but data support a putative role
for interleukin-1α (IL-1α). Factors causing increased sebaceous
secretion (puberty, hormonal imbalances) influence the eventual size of the
follicular plug. The plug enlarges due to accumulation of shed keratin and
sebum behind a very small follicular orifice at the skin surface with no
obvious opening and becomes visible as a closed comedone. An open comedone
(blackhead) occurs if the dilated follicular orifice opens. Further increase in
the size of a blackhead continues to dilate the pore, but usually does not
result in inflammation. The closed comedone is the precursor of inflammatory
acne papules, pustules, and nodules.
Hormonal Influences on Sebum Production and Composition
The
sebaceous gland is controlled primarily by androgens, with additional
influences from other hormones and neuropeptides. Androgens are produced both
outside the pilosebaceous unit, mainly by the gonads and adrenal glands, and
locally within the sebaceous gland via the action of androgen-metabolizing
enzymes such as 3β-hydroxysteroid dehydrogenase
(HSD), 17β-HSD and 5α-reductase.
Androgen receptors, found in the cells of the basal layer of the sebaceous
gland and the outer root sheath of the hair follicle, are responsive to
testosterone and 5α-dihydrotestosterone (DHT),
the most potent androgens. DHT has a 5–10-fold greater affinity than
testosterone for the androgen receptor and is thought to be the principal
androgen mediating sebum production.
A = androstenedione; ACTH = adrenocorticotropin-stimulating hormone; DHEAS = dehydroepiandrosteronesulfate; E = estrogen; FSH = follicle-stimulating hormone; LH = luteinizing hormone; T = testosterone; DOC = deoxycortisol.
Pathways of C19 steroid metabolism
Dehydroepiandrosterone
(DHEA) is a weak androgen that is converted to the more potent testosterone by
3β-hydroxysteroid dehydrogenase (HSD) and 17β-HSD in peripheral tissues like pilosebaceous
follicles. Finally, testosterone gets converted to dihydrotestosterone (DHT) by
5α reductase before it binds androgen receptors in target tissues,
predominantly on the sebaceous gland. Both DHEA and testosterone can be
metabolized to estrogens by the enzyme aromatase. The sebaceous gland expresses
each of these enzymes.
The
impact of androgens on sebaceous gland activity begins during the neonatal
period. From birth until approximately 6–12 months of age, infant boys have
elevated levels of luteinizing hormone (LH), which stimulates testicular
production of testosterone. In addition, both male and female infants exhibit
increased levels of dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEAS)
secondary to a large, androgen-producing “fetal zone” in the adrenal gland that
involutes during the first year of life. Of note, sebaceous gland activity in
infants is not due to persistent maternal hormonal stimulation, as was
previously hypothesized. Both testicular and adrenal androgen production
decrease substantially by 1 year of age and remain at a stable nadir until
adrenarche.
With
the onset of adrenarche, typically at 7–8 years of age, circulating levels of
DHEAS begin to rise due to its production by the adrenal gland. This hormone
can serve as a precursor for the synthesis of more potent androgens within the
sebaceous gland. The rise in serum levels of DHEAS in prepubescent children is
associated with an increase in sebum production and often the initial
development of comedonal acne. Although the overall composition of sebum is
similar in persons with or without acne, those with acne have variable degrees
of seborrhea and their sebum tends to have higher levels of squalene monounsaturated
fatty acids but less linoleic acid.
Little
is known about the physiologic role of estrogens in modulating sebum
production. Estrogen administered systemically in sufficient amounts decreases
sebum production, although the dose of estrogen needed is greater than the
dose required to suppress ovulation and increases the risk of thromboembolic
events. However, acne often responds to treatment with lower-dose oral
contraceptives containing 20–50 mcg of ethinylestradiol or its esters, because
suppression of ovulation itself inhibits ovarian androgen production.
Postulated mechanisms for estrogen-mediated downregulation of sebogenesis
include direct opposition of androgens within the sebaceous gland, a negative
feedback loop that decreases androgen production via inhibition of pituitary
gonadotropin release, and regulation of genes that affect sebaceous gland
activity.
Inflammation in Acne
It
is clear that when a follicle involved with acne ruptures, it exudes keratin,
sebum, P. acnes, and cellular debris into the surrounding
dermis, thereby significantly intensifying inflammation. However, inflammation
is also seen early in acne lesion formation. For example, in acne-prone sites,
the number of CD4+ T cells and levels of IL-1
have been shown to be increased perifollicularly prior to hyperkeratinization.
In addition, insulin-like growth factor-1 has been found to increase the
expression of inflammatory markers and sebum production in sebocytes.
The
type of inflammatory response determines the clinical lesion seen. If
neutrophils predominate (typical of early lesions), suppuration occurs and a
pustule is formed. Neutrophils also promote the inflammatory response by
releasing lysosomal enzymes and generating reactive oxygen species; levels of
the latter in the skin and plasma may correlate with acne severity. An influx
of lymphocytes (predominately T helper cells), foreign body-type giant cells,
and neutrophils results in inflamed papules and nodules. The type of
inflammatory response also plays a role in the development of scarring. Early,
nonspecific inflammation results in less scarring than does a delayed, specific
inflammatory response.
Propionibacterium acnes and the Innate
Immune System
P.
acnes is a Gram-positive, anaerobic/microaerophilic rod that is
found deep within the sebaceous follicle, often together with smaller numbers
of P. granulosum. In adults, P. acnes is the predominant organism in the
microbiome of the face and other sebaceous skin. P. acnes produce porphyrins (primarily
coproporphyrin III) that fluoresce with Wood’s lamp illumination.
For
the most part, P. acnes is considered to be a
commensal organism of the skin rather than a pathogen per se. Although studies have documented increased
levels of P. acnes on the facial skin of
acne patients, the P. acnes density
does not correlate with clinical severity. Because P. acnes is nearly ubiquitous yet not everyone has
acne, differences in the pathogenicity of particular P. acnes strains and variable host responses
to P. acnes have been postulated. In a comparison of
the microbiome of facial skin in individuals with and without acne, certain
ribotypes of P. acnes (types 4 and 5) are
more frequently found in acne patients, suggesting that these strains are
either more capable of inducing acne or better suited to survive in an acne
environment. However, another study showed that monocytes from the peripheral
blood of patients with acne exhibited more robust cytokine release in response
to P. acnes stimulation than did monocytes from
individuals without acne.
The pathogenicity of P. acnes includes the direct release of lipases,
chemotactic factors, and enzymes that contribute to comedo rupture, as well as
stimulation of inflammatory cells and keratinocytes to produce proinflammatory
mediators and reactive oxygen species. Lipases hydrolyze
sebum triglycerides to form free fatty acids, which are comedogenic and primary
irritants. Chemotactic factors attract neutrophils to the intact follicular
wall. Neutrophils elaborate hydrolases that weaken the wall. The wall thins,
becomes inflamed (red papule) and pustule, and ruptures, releasing part of the
comedone into the dermis. An intense, foreign-body granulomatous reaction
results in the formation of the acne nodule.
Interactions
between the skin’s innate immune
system and P. acnes play an important
role in acne pathogenesis. One mechanism is via Toll-like receptors (TLRs), a
class of transmembrane receptors that mediates the recognition of microbial
pathogens by immune cells (monocytes, macrophages, and neutrophils) as well as
by keratinocytes. TLR2, which recognizes lipoproteins and peptidoglycans as
well as CAMP factor 1 produced by inflammatory strains of P. acnes, is found on the surface of macrophages
surrounding acne follicles. P. acnes have
also been shown to increase expression of TLR2 and TLR4 by keratinocytes.
Through activation of the TLR2 pathway, P. acnes stimulates
the release of proinflammatory mediators such as IL-1α,
IL-8, IL-12, tumor necrosis factor-α [TNF-α], and matrix metalloproteinases. IL-8 leads to
neutrophil recruitment, the release of lysosomal enzymes, and subsequent
disruption of the follicular epithelium, while IL-12 promotes Th1 responses.
P.
acnes has also been shown to activate the NOD-like receptor
protein 3 (NLRP3) of inflammasomes in the cytoplasm of both neutrophils and
monocytes, resulting in the release of proinflammatory IL-1β. In addition, recent studies have shown that P. acnes stimulate Th17 responses in acne lesions.
Lastly, P. acnes can induce monocytes to differentiate
into two distinct innate immune cell subsets: (1) CD209+ macrophages, which more effectively
phagocytose and kill P. acnes and
whose development is promoted by tretinoin; and (2) CD1b+ dendritic cells that activate T cells and
release proinflammatory cytokines.
Mechanisms leading to high sebum production
1.
Excessive androgen production
2.
Increased availability of free androgen which
may be associated with a relative reduction of sex hormone binding globulin
(SHBG)
3.
An amplified target response mediated through
the conversion of testosterone to more active dihydrotestosterone
4.
An increased capacity of the intracellular
receptor to bind androgens
Clinical features
Types of Acne Lesions
1.
Active lesions (increasing severity)
1.
Microcomedone (may not be clinically
apparent)
2.
Open comedone (blackhead)
3.
Closed comedone (whitehead)
4.
Papule
5.
Pustule
6.
Nodule
7.
Pseudo-cyst
2.
Sequelae
1.
Post‐inflammatory
macular erythema
2.
Dyspigmentation (usually hyper pigmentation)
3.
Scarring
Acne is a
polymorphic, inflammatory disease of the skin which occurs in sites with well-developed
sebaceous glands, most commonly on the face (in 99% of cases) and to a lesser
extent on the back (60%) and chest (15%), also on the neck and upper arms. On
the trunk, lesions tend to be concentrated near the midline. Although one type
of lesion may predominate, close inspection usually reveals the presence of
several types of lesions. Seborrhea is a frequent and distressing feature. Despite evidence that inflammation is present in even the
earliest comedones, acne lesions are divided into non-inflammatory and
inflammatory groups based upon their clinical appearance.
Non-inflamed lesions
are the earliest lesions to develop in younger patients and embrace both open
(blackheads) and closed (whiteheads) comedones. The open comedo appears as flat
or slightly raised lesion, <5
mm in diameter with a conspicuous central, dilated follicular opening
that is filled with an inspissated core of shed keratin and lipid. Melanin
deposition and lipid oxidation within the debris may be responsible for the
black coloration. They frequently appear in a mid-facial distribution and when
evident early in the onset of the disease indicate a poor prognosis. Closed
comedones or whiteheads are generally <5 mm
in diameter; dome-shaped; smooth; skin-colored,
whitish, or greyish papules and have no visible follicular opening or
associated erythema. These lesions are often inconspicuous and better
appreciated upon palpation, stretching or side-lighting of the skin. Most
patients have a mixture of lesions. Comedones are required for diagnosis of any
type of acne.
There are also
several subtle subtypes of comedones whose presence may influence response to
therapy:
• ‘Sandpaper’
comedones consist of multiple, very small whiteheads, frequently distributed on
the forehead, which produce a roughened, gritty feel to the skin.
• ‘Macrocomedones’
are large whiteheads or occasionally blackheads greater than 1 mm in diameter.
Both macro comedones and sandpaper comedones respond poorly to conventional
topical treatments.
• ‘Submarine’
comedones are large comedonal structures greater than 0.5 cm in diameter and
are resident more deeply in the skin; they are frequently the source of
recurrent inflammatory nodular lesions.
• Secondary comedones
may be produced after exposure to dioxins (chloracne), pomades (pomade acne),
topical steroids and other drugs (drug-induced acne).
Inflammatory
acne is characterized by papules, pustules, and nodules of varying severity. Inflammatory
lesions arise from microcomedo or noninflammatory lesions and can develop into
superficial or deep lesions. The superficial lesions are usually papules and
pustules (5 mm or less in diameter), and the deep lesions are nodules and pseudocysts.
Erythematous papules typically range from 1 to 5 mm in diameter. Pustules tend
to be approximately equal in size and are filled with white purulent material
and normal flora, including P. acnes. As the severity of lesions progresses,
nodules form and become markedly inflamed, indurated
and tender. Nodules are seen more frequently in males. Nodules may
become suppurative or hemorrhagic. Suppurative nodules are called cysts
because of their resemblance to inflamed epidermal cysts. But they are not true
cysts (pseudo-cyst) because they are not lined by an epithelium. These pseudocysts are deeper and filled with a combination
of pus and serosanguineous fluid. Recurring rupture and re-epithelisation
of cysts results in epithelial-lined sinus tracts.
Scarring can be a complication of both non
inflammatory and inflammatory acne. Scars may show increased collagen
(hypertrophic scars and keloids) or be associated with loss of collagen (i.e.
ice-pick scars, rolling and box scar).
Ice-pick
scars are small, narrow, deep scars that are widest at the surface of the skin
and taper to a point in the dermis, most evident on the cheeks. Ice-pick
scarring can result from comedones alone. Rolling scars are shallow, wide scars
that have an undulating appearance. Box scars are wide sharply demarcated
scars. Unlike ice pick scars, the width of the box scars is similar at the
surface and base.
Complications
Almost all acne
lesions leave a transient macular erythema after resolution. In darker skin
types, post-inflammatory hyper pigmentation persists for months after
resolution. In some individuals, acne lesions may result in permanent scarring.
Early treatment of acne is essential for the
prevention of lasting cosmetic disfigurement due to scarring.
Prognosis and clinical
course
The age of onset of
acne varies considerably. It may start as early as 8 years of age or it may not
appear until the age of 20 or later. The course is one of several years
duration followed by spontaneous remission in majority of cases. While most
patients will clear by mid-twenties (25 years), some have acne extending well
into the third or fourth decades. About 70% of women complain of a flare 2–7
days premenstrual. Possibly, flaring is related to a premenstrual change in the
hydration of the pilosebaceous epithelium. It is shown that prepubescent
females with comedonal acne and those females with high DHEAS levels are predictors
of severe nodular acne.
ACNE
VARIANTS
Gram-negative
folliculitis
Gram-negative
folliculitis can occur as a complication of long term oral or, less frequently,
topical antibiotic therapy used to treat acne due to an increased carriage rate
of gram-negative rods in the anterior nares. Patients usually give a history of
initial success with oral tetracyclines followed by a worsening of their acne.
Clinical features include a sudden eruption of multiple, small follicular
pustules or occasionally nodular lesions, most frequently localized around the
perioral or perinasal regions. Cultures of these lesions and the anterior nares
reveal Escherichia aerogenes, Proteus mirabilis, Klebsiella pneumoniae,
Escherichia coli, Serratia marcescens, or Pseudomonas aeruginosa. These
organisms replace the Gram positive flora of the facial skin and mucous
membranes.
Discontinuation of
the current antibiotic is required; treated with either ampicillin (250 mg four
times a day) or trimethoprim (600 mg/day). However, the response may be slow
and relapse is almost inevitable. Isotretinoin is now considered the treatment
of choice (1 mg/kg/day for 20 weeks); relapse following oral isotretinoin being
much less likely.
Drug-induced acne
Some drugs may cause acneform
reactions; these account for about 1% of all drug‐induced skin eruptions. Clinically,
it is characterised by an abrupt onset of monomorphic eruption of
inflammatory papules and pustules, usually pruritic and follicular, in contrast to the heterogeneous morphology of
lesions seen in acne vulgaris. Lesions are seen primarily seen on the chest and back.
Comedones are usually
absent unless androgens are the cause.
The interval between drug exposure and the acneiform eruption depends on
the offending agent. This
explains why some clinicians use the term “folliculitis”.
Major
drugs implicated in acneiform eruptions include glucorticoids, androgens/ anabolic
steroids (danazol, testosterone), hydantoins,
lithium, isoniazide, high dose of vitamin B complex, halogenides like
bromides and iodides, and oral contraceptives (more
often those that contain progestins with androgen-like effects). Less commonly,
azathioprine, quinidine, and adrenocorticotropic hormone are the culprits. With
the introduction of EGFR and MEK inhibitors, drug-induced follicular eruptions
are increasingly seen by dermatologists.
|
CAUSES OF DRUG-INDUCED
ACNE |
||||
|
Common |
Uncommon |
|||
|
Anabolic steroids (e.g.
danazol, testosterone) |
Azathioprine |
|||
|
Bromides* |
Cyclosporine |
|||
|
Corticosteroids |
Disulfiram |
|||
|
Corticotropin |
Ethosuximide |
|||
|
EGFR inhibitors |
Phenobarbital |
|||
|
Iodides† |
Propylthiouracil |
|||
|
Isoniazid |
Psoralen + ultraviolet A |
|||
|
Lithium |
Quinidine |
|||
|
MEK inhibitors (e.g.
trametinib) |
Quetiapine |
|||
|
Phenytoin |
TNF inhibitors |
|||
|
Progestins |
Vitamins B6 and B12 |
|||
* Found in
sedatives, analgesics and cold remedies.
† Found in contrast dyes, cold/asthma
remedies, kelp, and combined vitamin–mineral supplements.
With iodides, in particular, inflammation may be marked. The iodine
content of iodized salt is low and, therefore, it is extremely unlikely that
enough iodized salt could be ingested to cause this type of acne.
Steroid acne
It
is also called ‘acne vulgaris in reverse’. In predisposed individuals, sudden
onset of follicular pustules and papules may occur approximately 2 weeks after
starting corticosteroids by any route (IV,
IM, oral, inhaled, topical). The pathology of steroid acne is that of a focal
folliculitis with a neutrophilic infiltrate in and around the follicle. The
lesions of steroid acne differ from those of acne vulgaris by being of uniform
size and symmetric distribution, usually on the neck, chest, and back. Post
inflammatory hyper pigmentation may occur, but comedones, pseucysts, and
scarring are unusual. The eruption
clears when steroids are discontinued. Topical therapy with benzoyl peroxide is
effective.
Histopathology
Histopathologic
examination of acne lesions demonstrates the stages of acnegenesis that
parallel the clinical findings. In early lesions, microcomedones are seen. A
mildly distended follicle with a narrowed follicular opening is impacted by
shed keratinocytes. The granular layer at this stage is prominent. In closed
comedones, the degree of follicular distension is increased and a compact
cystic structure forms. Within the cystic space, eosinophilic keratinaceous
debris, hair, and numerous bacteria are present. Open comedones have broad,
expanded follicular ostia and greater overall follicular distension. The
sebaceous glands are typically atrophic or absent. A mild perivascular
mononuclear cell infiltrate encircles the expanding follicle.
As the follicular epithelium distends, the cystic contents inevitably begin to rupture into the dermis. The highly immunogenic cystic contents (keratin, hair and bacteria) induce a marked inflammatory response. Neutrophils first appear, creating a pustule. As the lesion matures, foreign body granulomatous inflammation engulfs the follicle and end-stage scarring can result.
Differential diagnosis
Acne is rarely
misdiagnosed. The commonest mistaken diagnosis is rosacea, which occurs in
older patients after the age of 30 years. Rosacea
favors the malar region, chin, and forehead; the presence of telangiectasias,
an absence of comedones, nodules or scarring and
a history of easy flushing can aid in diagnosis. Rosacea patients may
also have ocular involvement, but rarely have truncal lesions. Some patients
appear to have features of both diseases and clinical acne may evolve into more
typical rosacea later in life.
In females, confusion
with perioral dermatitis is possible, but in these patients the lesions itch,
the skin is dry and there are no comedones.
Whiteheads (closed
comedones) may be confused with milia. Milia represent subepidermal keratin cysts
predominantly infraorbital in distribution. They are very common and can occur
in association with, although unrelated to, acne.
Pityrosporum folliculitis
presents on the upper trunk as moderately ill-defined, superficial plaques,
among which are scattered many papules or pustules. It is likely to be a host
reaction to M. furfur, which is a normal skin commensal.
TREATMENT
General principles of acne treatment
Acne management aims
to alleviate symptoms; clear existing lesions and limit disease activity so
preventing new lesions and scars developing and avoid negative impact on
quality of life. Most cases of acne clear spontaneously as the patient matures
through adolescence into adulthood; however, even mild cases can persist for
4–6 years and in severe cases the natural history could be in excess of 12
years. Patients should be reassured that there are treatments available that
can significantly limit the disease duration, but should be informed that
response is slow and resolution is directly linked to good adherence.
A
thorough history and physical examination are key to developing an appropriate
and maximally effective treatment plan. The physician should review with the
patient all prescription and over-the-counter medications used for acne or
other conditions, and note the clinical responsiveness to them. A review of
cosmetics, sunscreens, cleansers, and moisturizers is also helpful. In female
patients, a menstrual and oral contraceptive history is important in
determining hormonal influences on acne. Some patients may report an
improvement following sun exposure while others experience an exacerbation.
|
HISTORY AND PHYSICAL
EXAMINATION OF THE ACNE PATIENT |
|
|
History |
Physical examination |
|
1. Sex 2. 3. Age 4. 5. Motivation 6. 7. Lifestyle/hobbies 8. 9. Occupation Current and previous treatments Use of cosmetics, sunscreens, cleansers, moisturizers Menstrual history Medications ·
Corticosteroids ·
Oral contraceptives ·
Anabolic steroids ·
Other (e.g. lithium, EGFR
inhibitors) Concomitant illnesses Family history (including severity of acne, polycystic ovary
syndrome, inflammatory disease) |
1. Skin type (e.g. oily versus dry) 2. Skin colour/photo type 3. Distribution of acne · Face (e.g. “T-zone”, cheeks, jaw line) · Neck, chest, back, upper arms 4. Overall degree of involvement (mild, moderate or severe) 5. 6. Lesion morphology · Comedones · Papules, pustules · Nodules, pseudocysts · Sinus tracts 7. 8. Scarring · Pitted · Hypertrophic · Atrophic 9. Post inflammatory pigmentary changes |
On
physical examination, lesional morphology should be assessed, including the
presence of comedones, inflammatory lesions, nodules, and pseudocysts.
Secondary changes such as scarring and post inflammatory pigmentary changes are
also important clinical findings. The patient’s skin colour and type can
influence the chosen formulation of a topical medication. For example, patients
with oily skin tend to prefer the more drying gels and lotions, whereas those
with drier skin types may prefer creams.
Treatment
of acne vulgaris
Treatment
goals include scar prevention, reduction of psychological morbidity, and
resolution of lesions. Grading acne based on lesion type and severity can help
guide treatment. Topical retinoids are effective in treating inflammatory and
non-inflammatory lesions by preventing comedones, reducing existing comedones,
and targeting inflammation. Benzoyl peroxide is an over-the-counter
bactericidal agent that does not lead to bacterial resistance. Topical and oral
antibiotics are effective as monotherapy, but are more effective when combined
with topical retinoids. The addition of benzoyl peroxide to antibiotic therapy
reduces the risk of bacterial resistance. Oral isotretinoin is approved for the
treatment of severe recalcitrant acne and can be safely administered using the
iPLEDGE program. After treatment goals are reached, maintenance therapy should
be initiated. There is insufficient evidence to recommend the use of laser and
light therapies.
GUIDELINES
OF CARE FOR THE MANAGEMENT OF ACNE VULGARIS (J AM ACAD DERMATOL 2016; 74:945-73)
Treatment algorithm for adolescents and young adults
* May be prescribed as
a fixed combination product or as separate component.
Recommendations for
topical therapies
Benzoyl peroxide or combinations with
clindamycin are effective acne treatments and are recommended as monotherapy
for mild acne, or in conjunction with a topical retinoid, or systemic
antibiotic therapy for moderate to severe acne
Benzoyl peroxide is effective in the
prevention of bacterial resistance and is recommended for patients on topical
or systemic antibiotic therapy. Topical antibiotic (eg, clindamycin) is
effective acne treatments, but is not recommended as monotherapy because of the
risk of bacterial resistance. Topical retinoids are important in addressing the
development and maintenance of acne and are recommended as monotherapy in
primarily comedonal acne, or in combination with topical or oral antimicrobials
in patients with mixed or primarily inflammatory acne lesions. Using multiple
topical agents that affect different aspects of acne pathogenesis can be
useful. Combination therapy should be used in the majority of patients with
acne. Topical adapalene and benzoyl peroxide can be safely used in the
management of preadolescent acne in children Azelaic acid is a useful
adjunctive acne treatment and is recommended in the treatment of post
inflammatory hyper pigmentation Topical dapsone 5% gel is recommended for
inflammatory acne, particularly in adult females with acne.
Recommendations for
systemic antibiotics
Systemic antibiotics are recommended in the
management of moderate and severe acne and forms of inflammatory acne that are
resistant to topical treatments
Doxycycline and minocycline are more
effective than tetracycline, but neither is superior to each other. Doxycycline
and lymecycline should be selected in preference to minocycline.
Although oral erythromycin and azithromycin
can be effective in treating acne, its use should be limited to those who
cannot use the tetracyclines (ie, pregnant women or children <8 years of
age). Erythromycin use should be restricted because of its increased risk of
bacterial resistance.
Use of systemic antibiotics, other than the
tetracyclines and macrolides, is discouraged because there are limited data for
their use in acne.
Trimethoprim-sulfamethoxazole and
trimethoprim use should be restricted to patients who are unable to tolerate
tetracyclines or in treatment-resistant patients
Systemic antibiotic use should be limited to
the shortest possible duration. Re-evaluate at 3-4 months to minimize the
development of bacterial resistance.
Monotherapy with systemic antibiotics is not
recommended Concomitant topical therapy with benzoyl peroxide or a retinoid
should be used with systemic antibiotics and for maintenance after completion
of systemic antibiotic therapy
Recommendations for
hormonal agents
Estrogen-containing combined oral
contraceptives are effective and recommended in the treatment of inflammatory
acne in females. Spironolactone is useful in the treatment of acne in select
females.
ACNE MANAGEMENT GUIDELINES
BY THE DERMATOLOGICAL SOCIETY OF SINGAPORE
Mild acne
Comedonal acne
Limited
data suggest that increasing concentrations of tretinoin cream (i.e., 0.01%,
0.025%, 0.05%, and 0.1%) are associated with increased efficacy but with an
increased rate of side effects. In comparison, adapalene 0.1% gel or cream
causes less irritation versus tretinoin and is as efficacious as tretinoin
cream.
Azelaic acid 20% is a mild comedolytic with
anti-inflammatory activity. It is safe and effective as a treatment and
maintenance option for women with adult acne. It can be used during
pregnancy and can be useful in patients with acne and PIH, as it induces
hypopigmentation in darker skin. BPO (2.5%, 5%,
and 10%) has anti-inflammatory, antibacterial, and mild comedolytic activities
and does not induce bacterial resistance. Lower concentrations of BPO
(2.5% or 5%) are preferred, as there is increased irritation with increasing
concentrations of BPO and without a significant increase in efficacy between
the 2.5% and 10% concentrations.
Mild Papulopustular acne
Recommended
treatment for mild papulopustular acne includes fixed-combination products
containing BPO (with clindamycin or adapalene) with or without topical
retinoid/azelaic acid. The topical fixed-combination products are
effective in the treatment of mild-to-moderate papulopustular acne and can be
used as monotherapy applied once-daily.
Moderate
papulopustular acne
Treatment
recommendations for moderate papulopustular acne include fixed combinations of
antibiotics and/or adapalene/BPO and/or topical azelaic acid. Treatment
duration with systemic antibiotics should not exceed 3 to 4 months. At Week 6
of therapy, the patient’s response to treatment should be assessed. The use of
oral antiandrogens as an alternative second-line treatment might be suitable
for some women with moderate papulopustular acne.
Severe Papulopustular acne
Treatment recommendations include the use of oral antibiotics, topical retinoid/azelaic acid, BPO, and oral antiandrogen combinations. Topical treatment alone is not recommended. Patients should be followed closely to monitor treatment response, and second-line therapy should be considered when treatment response is inadequate after a suitable amount of time. Some doctors combine oral contraceptives with systemic antibiotics; however, there is insufficient data on the potentially superior efficacy of this approach.
Nodulocystic and conglobate acne
For these types of acne, oral
isotretinoin is the recommended treatment. For
severe nodular/conglobate acne a high dosage of oral isotretinoin of ≥0.5 mg/kg
can be recommended (120 to 150mg/kg cumulative dose). For
severe papulopustular or moderate nodular acne, 0.3 to 0.5mg/kg for six months can
be recommended. A daily dose of 0.25 to 0.5mg/kg
can be started and adjusted as tolerated. Pulse therapy (every 1 to 3 weeks) is
not recommended due to higher relapse rates. Low-dose maintenance for
persistent acne in adults can be considered, but with caution due to the
potential for adverse events (e.g., teratogenicity, hepatotoxicity,
hyperlipidemia). Lastly, combination with oral tetracyclines should be avoided
due to the risk of pseudotumour cerebri.
·
COCs are
effective for noninflammatory and inflammatory acne. They may be considered
alternatives to systemic antibiotics or systemic retinoids for
moderate-to-severe papulopustular acne in women, in combination with topical
retinoids with or without BPO.
|
TIPS FOR TOPICAL ACNE
THERAPY |
|
|
Improve adherence – often compromised due to patients having busy schedules
or quitting when the response is not rapid |
· Simplify the regimen: once daily when possible; consider
combination products (e.g. benzoyl peroxide + adapalene or clindamycin; adapalene
+ clindamycin), especially in less motivated adolescents · Inform patients that it will take 6–8 weeks of treatment for
substantial improvement · Ask specifically about adherence: “Out of 7 nights, how many
times do you apply the medication?” |
|
Educate on proper use |
· In general, topical medications (especially retinoids) should be
used to the entire acne-prone region rather than as “spot treatment” of
individual lesions · Provide instructions on where to apply the medication and how
much to use |
|
Minimize irritation – most common in adolescents with atopic dermatitis and
adults |
· Note that using too much medication or applying it too
frequently can increase irritation · Devise a gradual initial approach to improve tolerance in
patients with sensitive skin; for example, a single agent may be used for the
first 2–3 weeks (starting every other day for retinoids), followed by slow introduction
of a second medication (e.g. transitioning from alternate days to daily) · Advise to avoid harsh scrubs and other irritating agents (e.g.
toners, acne products that are not part of the regimen) · Suggest use of a non-comedogenic sensitive skin moisturizer if
dryness occurs |
|
Avoid exacerbation |
· Review all skin care products and cosmetics; having patients
bring everything that they apply to their face to a visit may help to
determine the source of problems · Advise non-comedogenic products (e.g. moisturizers, sunscreens,
make-up) and to avoid having oily hair or using pomades that may contribute
to acne. · Instruct patients not to pick or manipulate lesions |
|
|
|
Choice of therapy
This is largely
determined by the severity and extent of the disease.
Patients with mild
acne usually receive topical therapy alone; patients with moderate acne receive
oral and topical therapies; patients with more severe acne should be started on
oral antibiotic therapy but the need to commence oral isotretinoin should be
considered early in the course of their disease and may well be used first line
in those patients demonstrating poor prognostic factors which are associated
with more severe disease, as outlined in Table.
Table Poor prognostic factors in acne
Family history
Early onset:
Mild facial comedones
Early and more severe sebum production
Early onset relative to menarche
Hyperseborrhoea
Site of acne:
Truncal
Scarring
Persistent
Mode of action of therapeutic agents
Acne severity grading
Comedonal
acne
Non-inflammatory
acne lesions consisting of open and closed comedones
Mild
inflammatory acne
Few comedones,
papules and pustules (<10), no nodules, no scarring
Moderate
inflammatory acne
Several
comedones, papules and pustules (10-40) and few nodules up to 5, mild scarring
Severe
inflammatory acne
Numerous
comedones, papules and pustules (>40), multiple nodules >5, scarring
Severity-based approach to treating acne
Comedonal acne
Clinical
presentation
The
earliest type of acne is usually noninflammatory comedones (“blackheads” and
“whiteheads”). It develops in the pre-teenage or early teenage years and is
caused by increased sebum production and abnormal desquamation of epithelial
cells. There are no inflammatory lesions because colonization with P. acnes
has not yet occurred.
Treatment
Closed
comedone acne (whiteheads) responds slowly. A large mass of sebaceous material
is impacted behind a very small follicular orifice. The orifice may enlarge
during treatment, making extraction by acne surgery possible. Comedones may
remain unchanged for months or evolve into a pustule or nodule.
Retinoids
are applied at bedtime (tazarotene, tretinoin, adapalene). The base and
strength are selected according to skin sensitivity. Tazarotene may be the most
effective and most irritating. Start with a low concentration of the cream or
gel (available in 0.05% and 0.1%) and increase the concentration if irritation
does not occur. Tretinoin and adapalene are equally effective. Start with Tretinoin
such as Retin-A Micro (0.04% or 0.1%) or adapalene gel. Medications are used
more frequently if tolerated. Add benzoyl peroxide or topical antibiotics or combination
medicines later to discourage P. acne and the formation of inflammatory
lesions. The response to treatment is slow and discouraging. Several months of
treatment are required. Large open comedones (blackheads) are expressed; many
are difficult to remove. Several weeks of treatment facilitate easier
extraction. Topical therapy may need to be continued for extended periods.
Mild inflammatory acne
Clinical
presentation
Mild pustular and
papular inflammatory acne is defined as fewer than 20 pustules.
Treatment
Benzoyl
peroxide, a topical antibiotic, or combination medicine and a retinoid are
initially applied on alternate evenings. The lowest concentrations are
initially used. After the initial adjustment period, the retinoid is used each
night and benzoyl peroxide or antibiotic is used each morning. The strength of
the medications is increased if tolerated. Oral antibiotics are introduced if
the number of pustules does not decrease. Topical therapy may require
continuation for extended periods.
Moderate-to-severe inflammatory acne
Clinical
presentation
Patients who have moderate-to-severe
acne (more than 20 pustules) are temporarily disfigured.
The
explosive onset of pustules can sometimes be precipitated by stress. There may
be few to negligible visible comedones. Affected areas should not be irritated
during the initial stages of therapy.
Treatment
Many
dermatologists will begin with a topical retinoid and combine it with a topical
antibiotic. Others will treat with twice-daily application of a topical
antibiotic, benzoyl peroxide, or combination medicine. Response to treatment
may occur in 2 to 4 weeks. Oral antibiotics (doxycycline or minocycline) are
used for patients with more than 10 pustules. Treatment should be continued
until no new lesions develop (2 to 4 months) and then should be slowly tapered.
If there are any signs of irritation, the frequency and strength of topical
medicines should be decreased. Irritation, particularly around the mandibular
areas and neck, worsens pustular acne.
A
retinoid can be introduced if the number of pustules and the degree of inflammation
has decreased. Start minocycline at full dosage if there is no response to
doxycycline after 3 months. Pustules are gently incised and expressed.
Injecting each pustule with a very small amount of triamcinolone acetonide
(Kenalog 2.5 to 5.0 mg/ml) can give immediate and very gratifying results.
Those
who have responded well may begin to taper and eventually discontinue oral
antibiotics.
Patients
who do not respond to conventional therapy may have lesions that are colonized
by gram-negative organisms. Cultures of pustules and nodules are obtained and
an appropriate antibiotic such as ampicillin is started. The response may be
dramatic.
Severe: Nodular acne
Nodular acne
is a serious and sometimes devastating disease that requires aggressive
treatment. The face, chest, back, and upper arms may be permanently mutilated
by numerous atrophic or hypertrophic scars. Patients sometimes delay seeking
help, hoping that improvement will occur spontaneously; consequently, the
disease may be quite advanced when first viewed by the physician.
Patients
with a few inflamed nodules can be treated by implementing a program similar to
that outlined for moderate-to-severe inflammatory acne. Oral antibiotics,
conventional topical therapy, and periodic intralesional Kenalog injections may
keep this problem under adequate control.
Extensive nodular
acne requires a different approach. There are three less common variants of
nodular acne—pyoderma faciale, acne fulminans, and acne conglobata.
Pyoderma
faciale
The illness typically
appears in the mid face of post adolescent women of 20–40 years of age. It is
reported to occur in the context of traumatic emotional experience with sudden
explosives eruption of pustules and nodules, which may be interconnected by
sinuses. Marked erythema and oedema are usually present. Comedones are usually
absent. There is often no preceding history of acne. Facial flushing frequently
precedes the exacerbation. As the name
implies, the eruption is usually confined to the face, involving the cheeks,
chin, nose and forehead. In contrast to acne fulminans, there are usually no
systemic symptoms.
The daily ingestion
of high-dose vitamin B supplements has also been reported to be associated with
the sudden onset of pyoderma faciale.
Cultures help to differentiate
this condition from gram-negative acne. Highly inflamed lesions can be managed
by starting isotretinoin and oral corticosteroids. A study reported effective
management with the following: Treatment was begun with prednisolone (1.0 mg/kg
daily for 1 to 2 weeks). Isotretinoin was then added (0.2 to 0.5 mg/kg/day
[rarely, 1.0 mg/kg in resistant cases]), with a slow tapering of the
corticosteroid over the following 2 to 3 weeks. Isotretinoin was continued
until all inflammatory lesions resolved. This required 3 to 4 months. None of the
patients had a recurrence. This group of patients were “flusher and blushers,”
and it was suggested that pyoderma faciale is a type of rosacea. The
investigators proposed the term rosacea fulminans.
Acne
fulminans
Acne
fulminans is the most severe form of acne and is characterized by the abrupt
development of nodular and suppurative acne lesions in association with
systemic manifestations. This uncommon
variant primarily affects boys 13–16 years of age. Patients typically have mild
to moderate acne prior to the onset of acne fulminans, when numerous
microcomedones suddenly erupt and become markedly inflamed. There is rapid
coalescence into painful, oozing, friable plaques with hemorrhagic crusts.
There may be confluent abscesses leading to ulcer formation. The lesions
predominate on the chest and back and heal with significant scarring.
Aseptic osteolytic bone lesions causing bone pain may accompany
the cutaneous findings in approximately 40% of patients; the clavicle and
sternum are most commonly affected, followed by the ankles, humerus and
iliosacral joints. Systemic manifestations include fever, arthralgias,
myalgias, hepatosplenomegaly and severe malaise. Erythema
nodosum may also arise in association with acne fulminans. Laboratory
abnormalities vary and include an elevated ESR, proteinuria, leukocytosis, and
anemia. Laboratory studies are not required to establish the diagnosis,
but their evolution may parallel the clinical course and response to therapy. The related synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO)
syndrome, which can accompany acne fulminans. Acne fulminans has also been
associated with late-onset congenital adrenal hyperplasia and anabolic steroid
use, including therapeutic testosterone.
Antibiotic therapy is not effective. Recommended treatment of acne fulminans includes prednisone
0.5–1 mg/kg/day as monotherapy for at least 2–4 weeks, followed by initiation
of low-dose isotretinoin (e.g. 0.1 mg/kg/day) after the acute inflammation
subsides; after at least 4 weeks of this combination, the isotretinoin dose can
be slowly increased and the prednisone tapered over a period of 1–2 months.
Paradoxically, an acne fulminans-like flare
occasionally develops during the first few weeks of isotretinoin therapy for
acne; this may be avoided by starting with a low dose of isotretinoin and
concomitant administration of oral corticosteroids at the first sign of a flare
or possibly pre-emptively in high-risk patients. Additional treatment options
for acne fulminans include topical or intralesional corticosteroids, TNF-α inhibitors, interleukin-1 antagonists, and
immunosuppressive agents (e.g. azathioprine, cyclosporine). Dapsone may be
particularly beneficial in the treatment of acne fulminans associated with
erythema nodosum
The main features of acne fulminans
|
Gender |
Male gender dominant |
|
Age |
13–22
years |
|
Pathogenesis |
Unclear |
|
Onset |
Acute
and sudden |
|
Localization |
Upper
chest and back, shoulders, face |
|
Clinical
picture |
Ulcerative
lesions covered with hemorrhagic crusts healing with scarring |
|
Laboratory
findings |
Leucocytosis,
increased erythrocyte sedimentation rate, anemia, proteinuria, microscopic
hematuria |
|
Response
to conventional antibiotic therapy |
Poor |
|
Treatments
of choice |
Systemic
corticosteroids combined with isotretinoin |
Acne
conglobata
This is a severe form
of nodular acne and affects men more often than women with no or little
systemic upset. This acne variant is part of the follicular occlusion tetrad
along with dissecting cellulitis of the scalp, hidradenitis suppurativa and
pilonidal cysts. Lesions usually occur on the trunk (chest and back) and upper
limbs and frequently extend to the buttocks. In contrast to ordinary acne,
facial lesions are not common. The condition often presents in the second to
third decade and may persist into the 40s and 50s. The involved areas contain a
mixture of multiple grouped comedones, papules, pustules, nodules, abscesses,
draining sinuses and scars, often both keloidal and atrophic.
The
association of sterile pyogenic arthritis, pyoderma gangrenosum,
and acne conglobata can occur in the context of an
autosomal dominant autoinflammatory disorder referred to as PAPA syndrome.
The main features of acne conglobata
|
Sex |
Males
affected more frequently than females |
|
Age |
18–30
years |
|
Pathogenesis |
Unclear |
|
Onset |
May
be an insidious onset with a chronic course on the background of previous
acne or an acute deterioration of existing inflammatory acne |
|
Localisation |
Face,
trunk and limbs extending to the buttocks |
|
Clinical
picture |
Deep‐seated
inflammatory lesions, abscesses and cysts, causing interconnecting sinus
tracts. Polyporous grouped comedones and, significant scarring |
|
Laboratory
findings |
Gram‐positive
bacteria producing secondary infection |
|
Response
to conventional antibiotic therapy |
Poor |
|
Treatments
of choice |
Oral isotretinoin alongside
systemic corticosteroids to reduce inflammation Systemic
antibiotics to treat secondary infection and reduce inflammation |
Differential diagnosis of acne fulminans and
acne conglobate
|
|
Acne fulminans |
Acne conglobata |
|
Gender |
Men |
Men |
|
Age |
Adolescence
(13–16 years) |
20–25
years |
|
Onset |
Sudden |
Slow |
|
Location |
Face,
neck, chest and back |
Trunk
and upper limbs, facial lesions are rare |
|
Clinical
features |
Hemorrhagic
ulcerations |
Nodules,
inflammatory cysts, grouped comedones |
|
Systemic
symptoms |
Very
common |
None |
Therapeutic
agents for treatment of acne
Topical acne therapies
Topical
agents should be applied to the entire affected area to treat existing lesions
and to prevent the development of new ones. The most widely used topical drugs
are benzoyl peroxide (BPO), retinoids, antibiotics and azelaic acid, either as
monotherapy or in combinations. Earlier it was suggested that topical retinoids
should be limited to the treatment of comedonal lesions because of potential to
aggravate inflammatory acne. It has now been shown that topical retinoids have
some anti-inflammatory activity and also impact on the microcomedo, which
represents the precursor of non-inflammatory and inflammatory lesions. As a
result of these findings, topical retinoids are now ideally combined with
antimicrobials and should be considered in treating acne from the onset of acne
management. Topical BPO, antibiotics or azelaic acid have predominantly anti-inflammatory
activity in acne and can be used safely in combination with topical retinoids,
with the exception of tretinoin which is inactivated if used simultaneously
with BPO.
Topical retinoids
Topical retinoids are versatile agents in the treatment of
acne. The
anti-acne activity of topical retinoids involves normalization of follicular
keratinization and corneocyte cohesion, which aids in the expulsion of existing
comedones and prevents the formation of new ones, making them useful against noninflammatory lesions. Topical
retinoids also have significant anti-inflammatory properties, making them somewhat useful in the treatment of inflammatory
lesions. Topical retinoids are indicated as monotherapy for noninflammatory
acne and as combination therapy with antibiotics to treat inflammatory acne. Additionally, they are useful for maintenance after
treatment goals have been reached and systemic drugs are discontinued. In
addition, concurrent use of a topical retinoid can enhance the efficacy of
benzoyl peroxide and topical antibiotics by increasing the penetration of the
latter medications into the sebaceous follicle. The enhanced penetration
results in a synergistic effect with greater overall drug efficacy and a faster
response to treatment. Topical retinoids used for acne include tretinoin,
adapalene and tazarotene. Overall,
adapalene is the best tolerated topical retinoid. Limited evidence suggests
that tazarotene is more effective than adapalene and tretinoin. There is no
evidence that any formulation is superior to another. Topical products that
combine tretinoin with clindamycin or adapalene with benzoyl peroxide are also
available. The fixed-dose adapalene
0.1%–benzoyl peroxide 2.5% combination gel is an efficacious and safe acne
treatment.
The most common side effect of topical retinoids is local
irritation resulting in erythema, dryness, peeling, and scaling. This tends to
peak after 2–4 weeks of treatment and improve with continued usage. Continual
topical application leads to thinning of the stratum corneum, making the skin
more susceptible to sunburn, sun damage, and irritation from wind, cold, or
dryness. Irritants such as astringents, alcohol, and acne soaps will not be
tolerated as they were previously; transient
application of a low-potency topical corticosteroid may be of benefit for
patients with significant irritation. Delivery systems have been developed to
permit a greater concentration of retinoid while decreasing irritancy,
primarily through controlled slow release, e.g. tretinoin impregnated into inert
microspheres or incorporated within a polyolprepolymer. An acne flare may occur
during the initial month of treatment with a topical retinoid, but resolves
spontaneously with continued usage. Although not true photosensitizers, if a
retinoid causes skin peeling or irritation, this may increase the user’s
susceptibility to sunburn. Appropriate use of sunscreens should therefore be
advised.
Tretinoin (all-trans-retinoic acid), a naturally occurring metabolite
of retinol, was the first topical comedolytic agent used for the treatment of
acne. To decrease the potential for irritation, treatment is often started with
a lower-concentration cream formulation of tretinoin and the strength later
increased. Alternate-night to every-third-night application may be necessary
initially, with increased frequency as tolerated. Because the standard generic
tretinoin formulation is photolabile, night-time application is recommended to
prevent early degradation; it is also inactivated by concomitant application of
benzoyl peroxide, so the two medications should not be used at the same time.
However, specialized microsphere formulations of tretinoin are not photolabile
and can be applied together with benzoyl peroxide without degradation.
Although
epidemiologic studies have not shown an increased risk of birth defects in
infants of mothers using topical tretinoin during the first trimester, sporadic
case reports of birth defects have been published. Because of this and the fact
that systemic retinoids are known teratogens, the use of topical tretinoin in
pregnancy is discouraged. That said, dietary intake of vitamin A has been shown
to have a greater influence on serum retinoid levels than facial application of
tretinoin.
The
synthetic retinoid adapalene is an
aromatic naphthoic acid derivative. In the skin, it primarily binds the
retinoic acid receptor γ (RARγ), whereas tretinoin binds to both RARα and RARγ. Although
animal studies have shown adapalene to have milder comedolytic properties than
tretinoin, it is also less irritating. Unlike tretinoin, adapalene is
light-stable and resistant to oxidation by benzoyl peroxide.
Tazarotene is
a synthetic acetylenic retinoid that, once applied, is converted into its
active metabolite, tazarotenic acid. Like adapalene, this metabolite
selectively binds RARγ but not RARα or RXR. Both daily overnight applications of
tazarotene and short contact therapy regimens have been shown to be effective
in the treatment of comedonal and inflammatory acne. Topical tazarotene has
been designated pregnancy category X, so contraceptive counseling should be
provided to all women of childbearing age who are prescribed this medication.
Like adapalene, it is light-stable and can be applied together with benzoyl
peroxide.
Application techniques
The
skin should be washed gently with a mild soap no more than two to three times
each day, using the hands rather than a washcloth. Special acne or abrasive
soaps should be avoided. To minimize possible irritation, the skin should be
allowed to dry completely by waiting 20 to 30 minutes before application of
retinoids. The retinoid is applied in a thin layer once daily. Medication is
applied to the entire area, not just to individual lesions. A pea-sized amount
is enough for a full facial application. Patients with sensitive skin or those
living in cold, dry climates may start with an application every other or every
third day. The frequency of application can be gradually increased to as often
as twice each day if tolerated. The corners of the nose, the mouth, and the
eyes should be avoided; these areas are the most sensitive and the most easily
irritated. Retinoids are applied to the chin less frequently during the initial
stages of therapy; the chin is sensitive and is usually the first area to
become red and scaly. Sunscreens should be worn during the summer months if
exposure is anticipated.
Response to treatment
1
to 4 weeks: During the first few weeks, patients may experience
redness, burning, or peeling. Those with excessive irritation should use less
frequent applications (i.e., every other or every third day). Most patients
adapt to treatment within 4 weeks and return to daily applications. Those
tolerating daily applications may be advanced to a higher dosage or to the more
potent solution.
Three
to 6 weeks: New papules and pustules may appear because comedones
become irritated during the process of being dislodged. Patients unaware of
this phenomenon may discontinue treatment. Some patients do not worsen and
sometimes begin to improve dramatically by the fifth or sixth week.
After
6 weeks:
Most patients improve by the ninth to twelfth week and exhibit continuous
improvement thereafter. Some patients never adapt to retinoids and experience
continuous irritation or continue to worsen. An alternate treatment should be
selected if adaptation has not occurred by 6 to 8 weeks. Some patients adapt
but never improve. Retinoids may be continued for months to prevent appearance
of new lesions.
Benzoyl
peroxide (BPO)
Benzoyl peroxide is
an over-the-counter bactericidal agent that comes in a wide array of
concentrations and formulations. No particular form has been proven better than
another. Benzoyl peroxide is unique as an antimicrobial because it is not
known to increase bacterial resistance. It is most effective for the
treatment of mild to moderate mixed acne when used in combination with topical
retinoids. Benzoyl peroxide may also be added to regimens that include
topical and oral antibiotics to decrease the risk of bacterial
resistance.
BPO is a potent bactericidal agent that rapidly destroys
both surface and ductal P. acnes and yeasts. The lipophilic nature of
BPO allows it to penetrate the pilosebaceous duct. Once applied to the skin it
decomposes to release free oxygen radicals with potent bactericidal activity in
the sebaceous follicles and anti-inflammatory action. Benzoyl peroxide causes a
significant reduction in the concentration of free fatty acids via its
antibacterial effect on P. acnes. BPO has only mild comedolytic activity
and reduces the number of non-inflamed lesions
by decreasing follicular hyperkeratosis, but it is less effective than
retinoids at disrupting the microcomedo.
It does not impact on sebum production. In contrast to topical
antibiotics, microbial resistance to benzoyl peroxide has not been reported.
Many preparations for all skin types are available and includes bar soaps,
washes and gels, in concentrations ranging from 2.5% to 10% as well as products
that combine benzoyl peroxide with clindamycin or adapalene.
As benzoyl peroxide is a bleaching agent, whitening of clothing
and bedding can occur. Development of irritant contact dermatitis to benzoyl
peroxide may occur, and this should be suspected in patients who develop marked
erythema with its use. Although rare, approximately 2% of patients develop
allergic contact dermatitis from benzoyl peroxide and must discontinue its use.
The sudden appearance of diffuse erythema and vesiculation suggests contact
allergy to benzoyl peroxide.
BPO is particularly effective when used in combination with other
therapies. The
combination of clindamycin/benzoyl peroxide (Benza-Clin) is superior for
inflammatory and non-inflammatory acne versus either ingredient used alone.
Principles of
treatment
Benzoyl
peroxide should be applied in a thin layer to the entire affected area. Most
patients experience mild erythema and scaling during the first few days of
treatment, even with the lowest concentrations, but adapt in a week or two. An
adequate therapeutic result can be obtained by starting with daily applications
of the 2.5% or 5% gel and gradually increasing or decreasing the frequency of
applications and strength until mild dryness and peeling occur.
Topical
antibiotics
Topical antibiotics
are used predominantly for the treatment of mild to moderate inflammatory or
mixed acne. In comedones they reduce the perifollicular lymphocytes which are
involved in comedogenesis. They also significantly reduce numbers and function
of P. acnes. Some topical antibiotics also have a direct anti-inflammatory
action via an antioxidant effect on leukocytes. They are sometimes used as
monotherapy, but are more effective in combination with topical retinoids. Clinical trials have demonstrated that
application twice a day is as effective as oral minocycline 50 mg taken twice
daily. Most solutions are alcohol-based and may produce some degree of
irritation. Clindamycin lotion or gel is a commonly used topical antibiotic;
however, resistance of >50% of P. acnes strains
to this molecule has been reported in some countries.
Because of the
possibility that topical antibiotics may induce resistance, it is recommended
that benzoyl peroxide be added to these regimens.
Azelaic acid
Azelaic acid is a naturally occurring dicarboxylic
acid found in cereal grains that has antikeratinizing, antibacterial, and antiinflammatory
properties, but is not sebosuppressive. The
cream formulation is approved by the U.S Food and Drug Administration (FDA) for
the treatment of acne vulgaris, but the gel has significantly better
bioavailability. It is available as a topical 20% cream, which has been
shown to be effective in inflammatory and comedonal acne, as well as a 15% gel
marketed for rosacea. By inhibiting the growth of P. acnes, azelaic acid
reduces inflammatory acne. Azelaic acid reduces comedones by normalizing the
disturbed terminal differentiation of keratinocytes in the follicle
infundibulum. The activity of azelaic acid against inflammatory lesions may be
greater than its activity against comedones. Its efficacy can be enhanced when it is used in
combination with other topical medications such as benzoyl peroxide 4% gel,
clindamycin 1% gel. Azelaic acid cream may be combined with oral antibiotics
for the treatment of moderate-to-severe acne and may be used for maintenance
therapy when antibiotics are stopped. It does not cause sun sensitivity. It
does not induce resistance in P. acnes. Azelaic acid is
applied twice daily and its use is reported to have fewer local side effects
than topical retinoids. In addition, it may help to lighten post inflammatory
hyperpigmentation.
Topical
nicotinamide
Topical nicotinamide
4% has anti-inflammatory actions and doesnot induce P. acnes resistance.
A comparison of 4% nicotinamide gel demonstrated it to be similar in efficiency
to 1% clindamycin gel.
Salicyclic
acid
Salicylic acid is a
widely used comedolytic and mild anti-inflammatory agent thus reducing both non-inflammatory and inflammatory acne
lesions. It is also a mild chemical irritant that works in part by
drying up active lesions. Salicylic acid is available in concentrations of up
to 2% in numerous delivery formulations, including gels, and washes. Side
effects of topical salicylic acid include erythema and scaling.
Topical
dapsone
Topical dapsone
5% gel is approved for the treatment of acne vulgaris as it has antibacterial
and anti-inflammatory properties. Although it is an antibiotic, it likely
improves acne by inhibiting inflammation. Of note, a temporary yellow–orange
staining of the skin and hair occasionally occurs with concomitant use of
topical dapsone and benzoyl peroxide. Unlike oral dapsone, there is no evidence
that the topical formulation causes hemolyticanemia or severe skin reactions.
It is mostly used for inflammatory acne in females.
Topical
steroids
Potent steroids such as
clobetasol propionate applied twice a day for 5 days can dramatically reduce
the inflammation in an active inflammatory nodule.
Selecting topical therapy
Patients with mixed
lesions should be prescribed therapy active against comedones, inflammatory
lesions and microcomedones from the outset. Given the fact that the microcomedo
is the precursor to inflammatory and non-inflammatory lesions, even patients
with predominantly inflammatory acne should be prescribed a topical retinoid as
part of their regimen. Topical therapy should be prescribed alone for mild
acne, in conjunction with appropriate oral acne therapy for moderate acne, and
as maintenance therapy after oral therapy has stopped.
Topical therapy may
be necessary for many years. It is also important to stress to the patient that
topical therapy should be applied to all areas of skin within the active site
and not just visible lesions as clinically normal looking skin in an acne-prone
site is likely to have many evolving microcomedones. The concept of acne
prevention must be stressed to the patient. In conclusion, combined topical
therapies should be used for patients with mild inflammatory acne. Topical
retinoids have anti-inflammatory and comedolytic activity which makes them
suitable for treatment of comedonal and mild to moderate inflammatory disease
and they should therefore be used at the onset of treatment combined with
topical or oral antimicrobials. Topical retinoids are also advocated in
conjunction with oral antibiotics in patients with moderate and severe acne and
as maintenance treatment after cessation of systemic treatment. Selecting
therapies that work synergistically and impact on as many etiological factors
as possible will enhance treatment success. Products that combine preparations should
in theory be more convenient for patients to use and so aid adherence.
An Open-label Extension Study was conducted
Evaluating Long-term Safety and Efficacy of FMX101 4% Minocycline Foam for
Moderate-to-Severe Acne Vulgaris. The study concluded that FMX101 4%
minocycline foam, a new topical treatment option for patients with moderate
to-severe acne and appears to be safe, effective, and well tolerated for up to
52 weeks of treatment.
Oral
Treatments
Antibiotics
Mechanism
of action
The
primary mechanism of action of antibiotics is suppression of the growth of
follicular populations of P. acnes, thereby reducing bacterial
production of inflammatory factors. Neutrophil chemotactic factors are secreted
during bacterial growth, and these may play an important role in initiating the
inflammatory process. Because several antibiotics used to treat acne can
inhibit neutrophil chemotaxis in vitro, they are thought to act as an anti-inflammatory
agent.
Long-term
treatment
Patients
may express concern about long-term use of oral antibiotics but experience has
shown that this is a safe practice. Routine laboratory monitoring of patients
who receive long-term oral antibiotics for acne rarely detects an adverse drug
reaction and does not justify the cost of such testing. Laboratory monitoring
should be limited to patients who may be at higher risk for an adverse drug
reaction.
Dosage
and duration
Better
clinical results and a lower rate of relapse after stopping antibiotics are
achieved by starting at higher dosages and tapering only after control is
achieved. Antibiotics are prescribed in divided doses; there is better
compliance with twice-a-day dosing. Antibiotics must be taken for weeks to be
effective and are used for many weeks or months to achieve maximum benefit.
Attempts to control acne with short courses of antibiotics, as is often tried
to prevent premenstrual flare-ups of acne, are usually not effective.
How long and what dose?
It has been stated
that 3 weeks is required before any obvious improvement is noted and that a
minimum of 3 months extending to 6 months in conjunction with topical therapy
is required to achieve maximum benefit. In patients with non-responding
disease, doubling the dose of minocycline to 200 mg/day is more effective than
continuing on an average dose of 100 mg. Daily doses of doxycycline (100 mg),
minocycline (100 mg) and lymecycline (408 mg) are said to be equally effective,
provided P. acnes is not resistant to doxycycline and lymecycline.
The higher the sebum
extraction rate the less well the patients responded to their systemic therapy.
It is hypothesized that this may be related to dilution of the antibiotic
within the intrafollicular duct and as a result of this suggested that when the
sebum excretion rate is greater than 2.5 μg/cm2 a higher daily dosage of
antibiotics might be required (lymecycline 600 mg, doxycycline and minocycline
200 mg). When prescribing higher doses of antibiotics patients and physicians
should be wary about increased adverse effects.
Systemic antibiotics in papulopustular acne
Oral antibiotics are
indicated for severe acne, moderate facial acne not responding to topical
therapies and/or extensive truncal acne. Response to systemic antibiotics
varies. Young males with marked seborrhea and truncal acne respond less well
than females with purely facial acne. Because of the potential for bacterial
resistance with the use of an oral antibiotic, it is recommended that benzoyl
peroxide be added to any regimen of oral antibiotics.
After individual treatment goals have been
met, oral antibiotics can be discontinued and replaced with topical retinoids
for maintenance therapy. Topical retinoids are sufficient to prevent relapses
in most patients with acne vulgaris, especially if the disease was originally
classified as mild or moderate. If the patient's acne was initially classified
as severe inflammatory, benzoyl peroxide with or without an antibiotic can be added
for maintenance therapy.
Cyclines (tetracycline, oxytetracycline, doxycycline, lymecycline,
minocycline) are the antibiotics of choice. These second‐generation
cyclines may aid adherence and of these lymecycline and doxycycline should be
used in preference to minocycline.
Doxycycline
Doxycycline
is a safe and effective medication. Studies of doxycycline (50 and 100 mg)
showed no significant difference between its clinical efficacy and that of
minocycline in treating acne. Doxycycline is less expensive than minocycline.
The incidence of photosensitivity is low but increases with increasing dose
levels.
Dosing
Start
at 100 mg once daily or twice daily and decrease the dosage once control is
obtained. Doxycycline can be taken with food.
Minocycline
Minocycline
(50-mg and 100-mg capsules and scored tablets; 55-mg, 65-mg, 80-mg, 105-mg, and
115-mg extended-release tablets) is a tetracycline derivative that has proved
valuable in cases of pustular acne that have not responded to conventional oral
antibiotic therapy. Minocycline is expensive; generic forms are available. The
enhanced efficacy of minocycline, a lipophilic derivative of tetracycline, may
be due to its greater penetration into the sebaceous follicle. Due to reports
of potential serious adverse effects, minocycline is not recommended as first
line therapy.
Dosing
The
usual initial dosage is 50 to 100 mg twice each day. The dosage is tapered when
a significant decrease in the number of lesions is observed, usually in 3 to 6
weeks. Solodyn is an extended-release minocycline. It is a once-daily tablet
prescribed on the basis of the patient’s weight to achieve a dose of
approximately 1 mg/kg.
Adverse effects
Minocycline
is highly lipid-soluble and readily penetrates the cerebrospinal fluid, causing
dose-related ataxia, vertigo, nausea, and vomiting in some patients. In
susceptible individuals, central nervous system (CNS) side effects occur with
the first few doses of medication. If CNS adverse reactions persist after the
dosage is decreased or after the capsules are taken with food, alternative
therapy is indicated. Penetration of the blood-brain barrier may cause
pseudotumor cerebri. Pseudotumor cerebri syndrome associated with minocycline
therapy is reported in daily doses of 50 to 200 mg. Symptoms are headache
(75%), transient visual disturbances (41%), diplopia (41%), pulsatile tinnitus
(17%), and nausea and vomiting (25%).
Drug
hypersensitivity syndrome (DHS) occurring within 3 months of treatment
initiation characterized by fever, malaise, arthralgia and a diffuse
exanthematous skin eruption. Systemic involvement may include pulmonary
eosinophilia and hepatitis. Early recognition and withdrawal of the agent is
essential, repeat exposure may result in recurrence of DHS within a few days.
A
blue-gray pigmentation of the skin, oral mucosa, nails, sclera, bone, and
thyroid gland has been found in some patients, usually those taking high
dosages of minocycline for extended periods. Skin pigmentation has been
reported in depressed acne scars, at sites of cutaneous inflammation, as
macules resembling bruises on the lower legs, and as a generalized
discoloration suggesting an off-color suntan. Pigmentation may persist for
long periods after minocycline has been discontinued. The consequences of these
deposits are unknown. Tooth staining (lasting for years) located on the incisal
one half to three fourths of the crown has been reported in adults, usually
after years of minocycline therapy. In contrast, tooth staining produced by
tetracycline occurs on the gingival third of the teeth in children treated
before age 7. Autoimmune hepatitis, serum sickness–like reactions, and
drug-induced lupus have been reported in rare instances.
A
lupus‐like reaction has also been reported occurring after 6–48
months of treatment. Patients are usually female and present with fever,
malaise and polyarthralgia. A cutaneous rash is not always evident but
urticaria, vasculitis and non‐specific erythema have all been reported. Some patients have
concomitant liver disease, which may occur in the absence of joint symptoms.
Serology for lupus is evident with a positive antinuclear antibody (ANA), along
with positive perinuclear antineutrophilic cytoplasmic antibodies (pANCA) and
raised C‐reactive protein. Severely deranged hepatic enzymes and
rarely liver damage requiring liver transplantation have also been reported.
Positive antihistone antibodies are rarely identified. The lupus‐like
reaction is reversible if the drug is withdrawn but abnormal serology may
persist. Minocycline should be avoided in patients with a personal or family
history of systemic lupus erythematosus. Before embarking on long‐term
minocycline it is advisable to check hepatic function and ANA at baseline and
to repeat hepatic function, ANA and pANCA every 3–6 months.
Macrolides
Erythromycin
or azithromycin prescribing for acne has increasingly fallen out of favor due
to the emergence of antibiotic‐resistant strains of P. acnes. If antibiotic therapy
is required in pregnancy, oral erythromycin is thought to be safe. The safest topical
therapies in pregnancy are topical BPO and Azelaic
acid. Erythromycin remains the preferred
option in children (8–12 years) as tetracylines are contraindicated due to
potential musculoskeletal problems and discoloration of permanent teeth.
Oral
azithromycin using intermittent dosing schedules (250 or 500 mg three times a
week) due to the long half‐life of 68 h has been reported to be effective for acne. It
should be discouraged as it is commonly used to treat a variety of systemic infections.
Systemic
antibiotics in the treatment of acne vulgaris: dosage and adverse effects.
|
Antibiotic tetracyclines |
Dosage |
Adverse effects |
|
Oxytetracycline |
500
mg twice daily, 30 min before food and not with milk; makes adherence to
medication problematic for some |
Common: gastrointestinal upset Rare:
onycholysis, photosensitivity, benign intracranial hypertension |
|
Lymecycline |
300–600
mg daily |
As
oxytetracycline but tolerated better |
|
Doxycycline |
100–200
mg daily |
As oxytetracycline Photosensitivity
(dose dependent) |
|
Minocycline |
100–200
mg daily |
Rare
but serious: headaches and dizziness associated with benign intracranial
hypertension, pigmentary changes, autoimmune hepatitis/lupus erythematosus‐like
syndrome |
|
Erythromycin |
500
mg twice daily |
Common:
gastrointestinal upset, nausea, diarrhea |
General
side effects of oral antibiotics
All
oral antibiotics for acne can produce mild adverse effects. How antibiotics
should be administered to achieve optimal therapeutic response whilst avoiding
antibiotic resistance. Suggestions include restricting the duration of
antibiotics courses, use of combination regimens from the onset of therapy,
utilization of BPO either to reduce the emergence of or to treat antibiotic‐resistant
strains of P. acnes
and avoidance of using chemically dissimilar antibiotics and regular switching
of antibiotics.
Antibiotic prescribing policies
|
Strategy
to avoid propionibacterial resistance emerging |
Comments |
|
Avoid
inadequate dose of topical and systemic antibiotics |
Use
oral antibiotics for 3 months in the first instance and only continue if
clinical improvement continues |
|
If
extending the duration of oral antibiotics, utilize combination therapy |
Combine
with an agent that reduces the likelihood of promoting antibiotic
propionibacterial resistance. e.g. benzoyl peroxide |
|
If
repeated courses of antibiotics are required and the initial clinical
response was favorable, reuse the same drug |
This will avoid multiple resistant strains emerging |
|
Avoid
prescribing different oral and topical antibiotics concomitantly |
This
will avoid multiple resistant strains emerging |
|
Consider
using non‐antibiotic antimicrobials
wherever possible |
These
do not promote resistant isolates and when used with antibiotics may achieve
more rapid efficacy and so reduce the duration of the antibiotic course |
|
Topical
benzoyl peroxide (BPO) can be used for 7 days between antibiotic courses |
BPO
is fully active against sensitive and resistant strains of P. acnes and able to
eradicate resistant isolates |
|
Remember
to check medical adherence |
Poor
adherence to antibiotic therapies promotes resistance |
Reasons to suspect poor response due to resistance to antibiotic
therapies
|
Reasons
to suspect possible antibiotic‐resistant
P. acnes |
Comments |
|
Failure
to respond to antibiotic therapy |
Confirm
good adherence to therapy |
|
Deterioration
in acne despite continuing antibiotic therapy |
Patients
often confirm initial good results |
|
History
of poor adherence |
This
is thought to lend itself to resistance emerging |
|
Multiple
courses of oral and topical antibiotics |
Particularly
when used as monotherapy |
Reasons to suspect poor response to treatment
|
Reason
for poor response to therapy |
Comments |
|
Poor
adherence to therapy |
Steadily
diminishing adherence may lead to relapse |
|
Presence
of relevant antibiotic resistant P.
acnes in patient complying to therapy |
Colonization
with resistant isolates from the start results in poor response, subsequent
colonization leads to relapse |
|
Development
of Gram‐negative folliculitis |
|
|
Incorrect
diagnosis |
See
section on Differential diagnosis |
|
Presence
of macrocomedones prior to starting isotretinoin |
This
can result in significant flare of acne |
|
Intolerance
to or side effects of treatment |
See
section on Adverse effects |
|
Inadequate
dose of antibiotics |
Patients
of high body weight or marked seborrhea may require a higher dose |
ENDROCRINE
ACNE
Acne
can be the presenting sign of the overproduction of androgens.
Women have three major sources of androgens: i ) the ovaries, stimulated by the pituitary hormones follicle-stimulating
hormone (FSH) and luteinizing hormone (LH), which produce small quantities of
androgens [dehydroepiandrosterone sulfate (DHEA-S) and testosterone] that can
be released per se in
the circulation or converted into estrogen by the enzyme aromatase, which is
present in the ovarian follicle cells. At this level, disorders of androgen
excess are represented by functional ovarian hyperandrogenism, whereas
androgen-secreting tumors occur rarely.
ⅱ)
The adrenal gland produces DHEA-S which can be metabolized in more potent
androgens such as androstenedione and testosterone; and
ⅲ)
the skin, which has all the enzymes required for converting the weak androgens
into strong androgens such as testosterone and DHT.
In sebaceous glands, the increased activity
of these enzymes sustains the major role of androgens in inducing skin lesions.
Thus persistent acne can be explained in adult women with high levels of
testosterone and DHEA-S, which are practically the most important hormones for
the diagnosis of endocrine acne.
What are the hormones implicated to have
a role in acne pathogenesis?
Androgens
Increased sebum production due to androgens activity at the pilosebaceous
follicle is a prerequisite for acne in all patients. High level of androgens or
end-organ sensitivity of pilosebaceous units to a normal level of androgens
leading to sebum hypersecretion and infundibular hyperkeratinization.
The pilosebaceous unit of the skin (sebaceous
glands and hair follicles) can synthesize androgens by local conversion of weak
androgens to potent ones. Androgen receptors and enzymes involved in androgen
biosynthesis are also present in the portion of follicle where plugging first
begins and that is how androgen may be involved in initiating the development
of the earliest lesion of acne and microcomedones. On the basis of these findings, anti-androgenic
hormonal therapy has been examined as a possible treatment of acne in women.
Endocrinal evaluation
in patients with suspected hormonal acne
Hormonal evaluation is not mandatory for those
who experience short bouts of onset and offset or those who respond well to
standard treatments. However, in the more resistant cases and for those who
fail to respond to conventional therapies, endocrinal evaluation is an
important tool to consider as well as in the following cases:
1. Late-onset acne (presenting in the third decade) (acne tarda)
2. Therapy-resistant acne (Acne not responding to conventional treatment)
3. Boys and girls with prepubertal acne
4.
Stress-exacerbated acne
5. History of Severe flare-ups before menstruation
6. Hyperandrogenism (Hirsutism, Androgenic alopecia, Marked seborrhea, menstrual irregularities
7.
Signs of virilization (clitiromegaly, deepened voices, and
masculine features)
8.
PCOS
9.
Signs of hyperinsulinemia (obesity in the trunks, skin tags, and
acanthosis
nigricans)
10.
Distribution of the acne lesions. It is well recognized that
hormonal acne concentrates in the lower third of the face along the chin and
jaw lines.
The
evaluation of patients suspected of having hyperandrogenism includes a thorough
history and physical examination; the age of the patient and pubertal status
are also important parameters. Prepubertal children, adolescent girls, and
women with signs of hyperandrogenism, hormonal evaluation is a
prerequisite for hormonal therapy. The patient should be off any OCs or any
other hormonal therapy for at least 1 month before testing and the ideal time
of testing would be during the menstrual period (day 1-3) and the collection
should be done in the morning, between 8 and 10 am.
Initial tests typically include serum levels of total and free testosterone,
DHEAS, and 17-hydroxyprogesterone. Patients with clinical findings suggestive
of hypercortisolism,
serum cortisol should be measured because in adrenal neoplasia, all layers of
adrenal cortex may be hyperactive resulting in a Cushingoid status. Fasting and postprandial insulin levels should be checked
for overweight and obese patients.
To
confirm the source of excess androgen, one should either do an ACTH stimulation
test or a dexamethasone suppression test. Ovarian source of excess androgen
will fail to respond to this test, whereas the adrenal androgen level would
increase following ACTH stimulation and decrease following dexamethasone suppression test. Imaging studies like ultrasound ovaries
(preferably performed in luteal phase) and adrenals are recommended to look for
any mass or cyst and computed tomography (CT)\ magnetic resonance imaging (MRI)
for further delineation of the mass, if there is any.
X-rays of the hand and wrist to evaluate bone age should be
obtained in prepubertal children. In
the presence of cutaneous markers for hyperinsulinemia, serum level of insulin
both fasting and postprandial should be measured to rule out
hyperinsulinemia which is an important association of PCOS and independently
can also play a hormonal role in acnegenesis.
There are various causes of hyperandrogenism
in females. Ovarian causes of hyperandrogenism are PCOS or ovarian tumors (benign
or malignant). Adrenal causes of hyperandrogenism are classical congenital
adrenal hyperplasia (CAH), non-classical adrenal hyperplasia (NCAH), and
adrenal tumors (benign or malignant). Of all causes, PCOS accounts for >90% of the
overall causes of hyperandrogenism in women.
An
elevated serum DHEAS or 17-hydroxyprogesterone level indicates an adrenal
source of excess androgen production. The degree to which levels of these
hormones are increased is then useful in discerning the etiology. DHEAS values
in the range of 4000–8000 ng/ml or 17-hydroxyprogesterone levels >3 ng/ml
may be indicative of congenital adrenal hyperplasia. Defects in adrenal
enzymes, most commonly 21-hydroxylase or (less often) 11-hydroxylase, lead to
this condition. Patients with severe deficiencies of these enzymes become
symptomatic during infancy, whereas those with partial deficiencies present in
adolescence. If the serum DHEAS is >8000 ng/ml, with or without an elevated
testosterone level, an adrenal tumor should be suspected.
If
the testosterone levels (total and free) are elevated and the DHEAS level is
relatively normal, an ovarian source is likely. Polycystic ovary syndrome
(PCOS) is the most common condition associated with an elevated serum
testosterone, with levels typically ranging from 100 to 200 ng/dl. An increased
LH/FSH ratio (>2–3) is also commonly observed.
Polycystic ovary
syndrome (PCOS) is the most common hormonal disorder in young women. In PCOS,
there is increased ovarian production of androgen. The predominant pathology in
PCOS is chronic anovulation because of continuous high level of estrogen.
Rotterdam criteria for PCOS need the presence of at least two out of three
findings, oligomenorrhea or amenorrhea (defined as
the presence of <8 menstrual cycles per year), hyperandrogenism (HA)
(clinical evidence of androgen excess) or hyperandrogenemia (biochemical
evidence of androgen excess), and polycystic ovaries on ultrasound (12 or more
follicles in one ovary, measuring 2-9 mm in diameter, or total ovarian volume
greater than 10 mm 3). Hyperinsulinemia is another feature that exists as a cofactor or an important
extrinsic factor in many cases of PCOS and raised insulin level helps theca
leutin cells to escape desensitization to increasing level of LH which potentiates
androgen synthesis. It also inhibits
the SHBG synthesis by the liver. Oral contraceptives
and metformin should be considered in these patients, especially obese
teenagers because it can restore ovulation and improve symptoms of
hyperandrogenism. In patients who have contraindications to or are unwilling to
take oral contraceptives, metformin is more effective in restoring the normal
menstrual cycle and thus reducing acne.
When
levels of serum testosterone exceed 200 ng/dl, an ovarian tumor should be
considered.
How often do you find abnormal hormonal levels in hormone-responsive acne
patients?
It is important to remember that many patients
with hormonal acne might not have a raised level of circulating testosterone in
their blood and that some women with raised androgen levels can still have
normal menstruation. This is primary because only a small portion of the
testosterone (1%–2%) is being free and able to bind to the androgen receptors
(ARs) to induce action, so unless free testosterone is measured separately,
total testosterone level may still be normal in spite of obvious
hyperandrogenism signs. Signs of hyperandrogenism despite normal levels of
both total and free testosterone can be explained by the fact that there is an
increased sensitivity of the receptors to androgen at the pilosebaceous unit or
an increased activity of the 5α-reductase enzyme resulting in overproduction of
DHT, which is five times more potent than testosterone.
Hormonal therapy for Acne
For those patients with
contraindication to other modes of therapy or to those women thinking of
contraception, hormonal treatments can also be of choice. However, hormonal
treatment is not indicated as monotherapy. In general terms, the
objectives of hormonal therapy in acne are to 1) suppress androgen production
from ovaries and adrenals and pituitary and 2) inhibit ARs on sebaceous glands.
The European guidelines on acne therapy
recommend hormonal treatment along with topical or systemic antibiotics in
severe papulopustular and moderate nodular acne cases as an alternative to
starting therapy with isotretinoin. In the nodular or conglobate type of acne,
antibiotics along with hormonal treatment are a recommendation of choice. In
the mildest type of acne (comedonal), it is absolutely contraindicated to use
hormones (Table 1)
Table
1
Summary of treatment
recommendations from the European acne guidelines
|
Type of acne |
First-line treatment |
Second-line treatment |
Third-line treatment |
Hormonal alternatives for women |
|
Comedonal acne |
Topical retinoids, adapalene is preferred to tretinoin |
Benzoyl peroxide (BPO) or azelaic acid |
– |
Not recommended |
|
Mild to moderate papulopustular acne |
BPO + adapalene or
BPO + clindamyci |
BPO or azelaic acid or systemic antibiotic + adapalene |
Oral isotretinoin; or systemic antibiotics + BPO; or
systemic antibiotics + azelaic acid; systemic antibiotics + adapalene + BPO |
Not recommended |
|
Severe papulopustular acne and mild nodular acne |
Systemic isotretinoin |
Systemic antibiotics + adapalene; systemic antibiotics +
azelaic acid; or systemic antibiotics + BPO + adapalene |
Systemic antibiotics + BPO |
Hormonal antiandrogens + topical treatment or systemic
antibiotics (topical treatment is preferred) |
|
Severe nodular acne and conglobate acne |
Systemic isotretinoin |
Systemic antibiotics + azelaic acid |
Systemic antibiotics + BPO; or systemic antibiotics +
adapalene; or systemic antibiotics + BPO + adapalene |
Hormonal antiandrogens + systemic antibiotics (consider as
third line treatment) |
Hormonal
therapy is an established second-line treatment for female patients with acne
and can be very effective, irrespective of whether or not the serum androgen
levels are abnormal. It
is frequently used as a combination and not a stand-alone therapy. It can be
synergistically combined with antibiotics, benzoyl peroxide, azelaic acid, and
even retinoids. A course of 3 months is often necessary before experiencing
much improvement and benefit from treatment. Drugs used in the hormonal
treatment of acne fall into four major categories: 1) AR blockers
(spironolactone, cyproterone acetate) act at the peripheral level (hair
follicle, sebaceous gland); 2) estrogens (oral contraceptives), suppressing androgen production by the
ovaries, 3) glucocorticoids (prednisone), suppressing adrenal androgen production, and
4) enzyme inhibitors (5α-reductase inhibitors; Table 2.
Table
2
Different hormonal therapies
and their mechanism of action and possible side effects
|
COC |
Spironolactone |
Cyproterone acetate |
||
|
Mechanism of action |
Decreases 5α-reductase activity |
Decreases |
Blocks testosterone receptors |
|
|
Side effects |
GI disorders |
Hypercalcemia |
Headache |
|
|
Contraindications |
Smoking in age >35 years |
Risk of estrogen-dependent malignancy |
History of meningioma |
Abbreviations: COC combined oral contraceptives; GI,
gastrointestinal; CVS, cardiovascular; BMI, body mass index.
Androgens in acne pathogenesis and the
countervailing effects of combined oral contraceptives (OCs) and antiandrogens
Gonadotropin stimulation of ovaries leads to increased
androgenesis. Testosterone is derived from ovarian and adrenal glands. Sex
hormone binding globulin (SHBG) binds to testosterone thereby reducing the
fraction available for biological activity. Conversion of testosterone to
dihydrotestosterone (DHT), the more potent tissue-active metabolite, is
mediated by 5α reductase in tissues. DHT increases sebum excretion from
sebaceous glands and induces epidermal hyperkeratinization at the infundibulum
of pilosebaceous units. These events lead to the formation of comedones.
Subsequent proliferation of P. acnes bacteria leads to inflammation, manifested
as inflammatory lesions of acne. Combined OCs act to block certain portions of
the androgenic pathway (X) and enhance
SHBG production (+). Antiandrogens, including Drospirenone,
induce androgen receptor blockade at relevant tissue sites (I).
Mechanism of action of combined OCs in acne
Combined OCs is comprised of estrogenic and
progestogenic components. Their antiandrogenic potential in acne results from a
variety of mechanisms (see Figure). Suppression of pituitary gonadotrophin
secretion reduces androgen production by the ovaries. Additionally, combined
OCs directly inhibits androgenesis by the ovaries and adrenal glands. The
estrogenic component of these agents increase hepatic production of sex hormone
binding globulin (SHBG) which binds to testosterone, thereby reducing levels of
bioavailable testosterone. The progestin component inhibits 5-α reductase
activity, reducing the conversion of testosterone at end-organs to the more
biologically potent dihydrotestosterone (DHT). Furthermore, some progestins act
as inhibitors to DHT and other androgens by competitive binding to androgen
receptors. Recent studies have shown that androgen receptors can be found at
the basal layer of sebaceous glands of the skin and that skin and sebaceous
glands contain the biochemical substrates for androgen production and
metabolism. Major isozymes of steroid metabolizing enzymes can be found in
human sebaceous glands and androgens can be produced within them from
adrenal-derived dehydroepiandrosterone sulfate. Accordingly, the antiandrogenic
effects of some progestins may also be mediated locally by inhibiting autocrine
stimulation of sebaceous glands by androgens.
This can be accomplished by using the following:
Suppressors
of ovarian androgen secretion
Combined
oral contraceptives (COCs)
Combinations of both estrogen and progestins reduce the
cutaneous androgen effect by exerting their action through negative feedback on the pituitary
gonadal axis by
suppressing gonadotropin release (luteinizing hormone), which results in
suppression of ovarian and adrenal androgen production. Progestins are included basically to avoid the
risk of developing endometrial cancer imposed by the unopposed estrogen action.
The estrogen component in combined oral
contraceptives (COCs) is almost always ethinyl estradiol. Although
progestins have intrinsic androgenic activity, second-generation progestins
(e.g. ethynodioldiacetate, norethindrone, levonorgestrel) have lower androgenic
potential. Newer, third-generation progestins (e.g. desogestrel, norgestimate,
gestodene) have even less androgenic activity than their predecessors, and
other progestins (e.g. drospirenone, cyproterone acetate, dienogest) have antiandrogenic properties. Drospirenone is the only progestin approved by
the Food and Drug Administration (FDA), which blocks the AR and is truly
antiandrogenic, even without the addition of estrogen.
Estrogens can inhibit androgens by several
mechanisms:
1.
Suppress secretion of pituitary gonadotropins, inhibit ovulation,
and thus inhibit androgen production by the ovaries.
2.
Block the AR.
3.
Estrogens act on the liver to increase
synthesis of sex hormone binding globulin (SHBG), which binds testosterone and
reduces the level of free circulating testosterone.
4.
Progestins contained in the COCs suppress 5α-reductase and thus
inhibit the formation of potent androgens.
COCs are the first line of treatment for women
presenting with PCOS. Oral contraceptives also regulate menstrual
cycles in oligomenorrheic women. It is administered from day 1 of menstrual
cycle and given in 21 days on/7 days off regimen, for 5-6 cycles, after
obtaining a negative pregnancy report.
Three oral contraceptives are currently FDA-approved for the
treatment of acne, although others also have evidence of efficacy. The first is
a triphasic oral contraceptive composed of a norgestimate–ethinyl estradiol
(35 mcg) combination. The second contains a graduated dose of ethinyl estradiol
(20–35 mcg) in combination with norethindrone acetate, while the third contains
a stable dose of ethinyl estradiol (20 mcg) plus drospirenone (3 mg).
Common
side effects, which usually subside after 2-3 months, are irregular
menstrual periods, nausea, vomiting, breast tenderness, and weight gain. Less
common side effects include decreased libido, melasma, and mood changes. Agents containing drospirenone can lead to
elevations in serum potassium levels, but this is generally not clinically
significant in otherwise healthy individuals. Rare but more serious
complications include hypertension and vascular thromboembolism (e.g. deep venous
thrombosis, pulmonary embolism). The risk of thromboembolism is increased three times
in users than nonusers of the pills. The increase in risk of thromboembolism ranges from 2–4-fold
with levonorgestrel or norethindrone to 3.5–7-fold with desogestrel,
drospirenone and cyproterone acetate, and risk of thrombosis is at
its highest during the first year of use. Overall the risk is highest for women over the age of 35 years,
smokers, and those with other prothrombotic risk factors such as hereditary
thrombophilia.
Based on WHO
recommendations, the use of COCs is absolutely contraindicated in pregnancy, personal or family history of
thromboembolism, liver disease, and in smokers aged ≥35 years, while relative
contraindications include breastfeeding, poorly
controlled hypertension, migraine, and existing
malignancies. Moreover, certain conditions might be worsened by contraceptives
such as insulin resistance and is contraindicated in diabetic patients,
clotting disorders, and in patients with increased risk of breast cancer
Dermatologists
can initiate an OC prescription with an advice to follow-up with a gynecologist
because a physical examination, including a pelvic examination might be
appropriate. In a recent publication, it is stated that
concomitant use of antibiotics such as tetracycline and doxycycline with OCs
does not interfere with contraceptive steroid levels. Although the effects of
OCs as monotherapy have been well established, they can be used in combination
with other topical and oral therapies for acne for better results.
Androgen receptor blockers
Spiranolactone
Spironolactone is an
androgen receptor antagonist with unclear effectiveness in the treatment of
acne. It is usually reserved as a second- or third-line agent or as an
alternative to isotretinoin for women who cannot use this medication. A 2009
systematic review found insufficient evidence to recommend the use of
spironolactone for the treatment of acne.
Spironolactone mediates
its action through the following:
1.
Nuclear blockage of ARs in a competitive action to testosterone
and DHT preventing their binding and actions.
2.
Decreasing testosterone formation by inhibiting Type 2 17B-HSD
enzyme (beta Hydroxysteroid dehydrogenase).
3.
Direct inhibition of 5α-reductase resulting in less DHT formation.
4.
Increasing the level of SHBG and hence decreasing the levels of
circulating testosterone.
In doses
of 50–100 mg twice daily after meal, it has been shown to reduce sebum
production and improve acne. Up to two-thirds of women treated with
spironolactone note marked improvement or clearance of their acne. Side effects
are dose dependent and include irregular menstrual periods, headache, fatigue,
breast tenderness, decreased libido and hypotension. It is a potassium-sparing diuretic and may cause severe
hyperkalemia. Hyperkalemia is an electrolyte imbalance that
should be monitored and checked periodically for those on spironolactone
therapy. Potassium monitoring should be done frequently and on regular
basis while on spironolactone and the drug should be immediately stopped in
hyperkalemia of concern. Because pregnancy is an absolute contraindication, as it can
cause hypospadias and feminization of male fetus, its use with OCs is
recommended. Since metrorrhagia is the most common adverse effects of
spiranolactone, its incidence can be significantly decreased by adding OCs to
the patient’s regimens. Side
effects can be minimized if therapy is initiated at a low dose (25–50 mg/day).
Effective maintenance doses range from 25 to 200 mg/day. As with other hormonal
therapies, a clinical response may take up to 3 months.
Guidelines for Treatment
of Acne with Spironolactone
Pre-treatment
evaluation
1.
Obtaining baseline blood pressure
Guidelines
for starting treatment
1.
Begin with 1 or 2 mg/kg/day (50-100 mg/day)
as a single daily dose to minimize side effects.
2.
Check serum potassium levels and blood
pressure in 1 month. Topical therapies and systemic antibiotics may be
continued while spironolactone treatment is initiated. Tapering of the standard
therapies may then be possible as a beneficial response to spironolactone is
noted.
3.
Oral contraceptives, if not contraindicated,
may be given concomitantly at the start of treatment with spironolactone, or
they can be considered if menstrual irregularities develop.
4.
If no clinical response is seen in 1 to 3
months, consider increasing the dosage to 150 or 200 mg/day as tolerated. Good
clinical responses can be followed by a reduction of the dosage to the lowest
effective daily dose.
5.
If adverse effects develop, consider lowering
the dose.
Cyproterone
acetate (CPA)
CPA exhibits the two
properties of being a potent androgen receptor blocker, and also has antiandrogen
progestin activity, and is used as the progestin in oral contraceptives. The standard contraceptive formulation combines cyproterone
acetate (2 mg) with ethinylestradiol (35). This preparation is widely used as
the treatment of choice for sexually active women with hormonally responsive
acne. In India, CPA is available in
combination with EE (e.g., Diane 35 containing 2 mg CPA with 35 μg EE), highly
effective in improving acne. The most frequent side
effects are breast tenderness, headache, nausea/vomiting, and irregular menses;
hepatotoxicity and thromboembolism represent uncommon complications.
Suppressor of adrenal androgen secretion
Corticosteroids
Corticosteroids can
be considered in recalcitrant cases of acne not responsive to oral
contraceptives or spironolactone and for patients with elevated DHEAS level.
Corticosteroids can be used alone or in combination with oral contraceptives
and antiandrogens. An elevated DHEAS level indicates adrenal androgen
overproduction. Deficiency
of 21 hydroxylase and less often eleven hydroxylase enzymes shifts the hormonal
production of the adrenals toward androgens instead of steroids. In such a case, a low-dose prednisone (2.5–5 mg)
or a low-dose dexamethasone (0.25–0.75 mg) once at bedtime is thought to
counteract the unopposed ACTH production of androgens. The risk of adrenal
suppression is greater with dexamethasone. Low-dose steroids administered at
bedtime prevent the pituitary from producing extra adrenocorticotropic hormone
(ACTH) and thereby reduce the production of adrenal androgens. This night time dose is thought to suppress the
early morning peak of ACTH and meanwhile inhibit androgen formation. The initial
dosage should be prednisone 2.5 mg, and the dosage should be increased to
prednisone 5.0 to 7.5 mg if the DHEAS level has not been decreased after 3 to 4
weeks of treatment. Therapy is continued for 6 to 12 months, but the benefits
may persist for a longer time. This low dosage produces a clinical improvement
and suppresses DHEAS levels. At these dosages, few patients experience shutdown
of the adrenal-pituitary axis or other adverse effects of the drug. ACTH
stimulation tests or determination of early morning cortisol levels may be
performed every few months to ensure there is no adrenal suppression. Not all
patients respond.
Monitoring long-term
side effects of steroids such as osteoporosis and blood sugar levels is
mandatory, and long-term use of >6 months is not preferred. The risk of
adrenal suppression should be tested every 2 months using the ACTH stimulation
test.
Insulin
sensitizer
Insulin resistance decreases uptake of insulin
by cells and results in increased levels of insulin. Insulin resistance plays
an important role by increasing the pool of androgens by the ovaries and
adrenals and by decreasing the synthesis of SHBG resulting in a state of
hyperandrogenemia. Metformin is used, especially in acne in association
with PCOS, HAIR-AN syndrome, obese patients, or biochemical evidence of
hyperinsulinemia, and it is important to note that metformin does not cause
hypoglycaemia. It is usually given in a dose of 500 mg OD to BD doses to
up to 2000 mg/day. There is no particular limit to duration of Metformin use, but it should be discontinued in 6 months if no
improvements are seen. Most side effects are
dose dependent and include nausea and vomiting, limiting its use to
postprandial intake and starting with a low dose of 250 mg. Pioglitazone
and rosiglitazone can also be used for similar purposes. These insulin
sensitizers may be used in combination with OCs.
ISOTRETINOIN
Isotretinoin is still the only treatment that has been shown to
induce long-term remissions and even “cure” acne, because it is the only
medication that affects, albeit not to the same degree or permanently, all the
etiologic factors implicated in acne: sebum production, comedogenesis, and
colonization with P. acnes. Oral isotretinoin
(13-cis-retinoic acid) is a FDA approved drug for patients with severe,
nodular acne refractory to treatment, including oral antibiotics. Over time,
other less severe clinical forms of acne that is treatment resistant have also
been shown to benefit greatly from the use of isotretinoin. These include
significant acne who has responded unsatisfactorily to conventional therapies
such as topical retinoids plus oral antibiotics and/or results in scarring, as
well as Gram-negative folliculitis, pyoderma faciale and acne fulminans. Isotretinoin
remains the most clinically effective acne therapy, producing long‐term
remission or significant improvement in many patients.
Guidelines for the
Treatment of Acne with Isotretinoin capsules
Indications
1.
Severe, recalcitrant nodular and inflammatory
acne
2.
Moderate acne unresponsive to conventional
therapy
3.
Patients who scar
4.
Excessive oiliness
5.
Severely depressed patients
Unusual variants
1.
Acne fulminans
2.
Gram-negative folliculitis
3.
Pyoderma faciale
Dosage
Total cumulative dose determines remission
rate
Cumulative
dose 120 to 150 mg/kg
1.
88% of patients have a stable, complete
remission when treated in this dosage range
2.
No therapeutic benefit from doses >150
mg/kg
3.
0.5 to 1.0 mg/kg/day for 4 months—typical
course of prescription
4.
Optimal long-term benefit: 1.0 mg/kg/day for initial
course of prescription
5.
1.0 mg/kg/day × 120 days = 120 mg/kg
Treat
with 1 mg/kg/day especially in
1.
Young patients
2.
Males
3.
Severe acne
4.
Truncal acne
Treat
with 0.5 mg/kg/day in
1.
Older patients, especially men
2.
Double dosage at end of 2 months if no response
Duration
1.
Usually 85% clear in 4 months at 0.5 to 1.0
mg/kg/day; 15% require longer prescription
2.
May treat at lower dosage for longer period
to arrive at the optimum total cumulative dosage
Relapse
1.
39% relapse (usually within 3 years, most
within 18 months)
2.
23% require antibiotics
3.
16% require additional isotretinoin
Additional courses of isotretinoin
1.
Appears to be safe
2.
Response is predictable
3.
Some patients require three to five courses
4.
Cumulative dosage for each course should not
exceed 150 mg/kg
Indications
Severe, recalcitrant nodular and inflammatory acne
A
few patients with severe disease respond to oral antibiotics and vigorous
drying therapy with a combination of agents such as benzoyl peroxide and
sulfacetamide/sulfur lotion. Those who do not respond after a short trial of
this conventional therapy should be treated with isotretinoin to minimize
scarring.
Moderate acne unresponsive to conventional therapy
Moderate
acne usually responds to antibiotics (e.g., doxycycline) plus topical agents.
Change to a different antibiotic (e.g., minocycline 100 mg twice daily) if
response is poor after 3 months. Change to isotretinoin if response is
unsatisfactory after two consecutive 3-month courses of antibiotics. Patients
who have a relapse during or after two courses of antibiotics are also
candidates for isotretinoin.
Patients who scar
Any
patient who scars should be considered for isotretinoin therapy. Acne scars
leave a permanent mark on the skin and psyche.
Excessive oiliness
Excessive
oiliness is disturbing and can last for years. Antibiotics and topical therapy
may provide some relief, but isotretinoin’s effect is dramatic. Relief may last
for months to years. Some patients respond to a long-term low-dose regimen such
as 10 mg every other or every third day.
Severely depressed or dysmorphophobic patients
Some
patients, even with minor acne, are depressed. They respond well to
isotretinoin, although some may relapse quickly and require repeat courses.
Dosage
The
severity of the side effects of isotretinoin is proportional to the daily dose.
Patients with acne are typically treated with an
isotretinoin dose of 0.5–1 mg/kg/day taken with a fatty meal to increase
gastrointestinal absorption, often with a lower dose during the first month of
treatment to prevent an initial acne flare and allow the patient to adjust to
dose-dependent side effects.
The
cumulative dose may be more important than the duration of therapy. A
cumulative dose of 120–150 mg/kg is associated with significantly better
long-term remission and reduces the risk of relapse. This
dosage level can be achieved by1 mg/kg/day for 4 months. However, a 6-month
course of low-dose isotretinoin (e.g. 0.25–0.4 mg/kg/day, 40–70 mg/kg
cumulative) can be effective in the treatment of moderate acne, with fewer side
effects and improved patient satisfaction. The therapeutic benefit from a total
cumulative dose of more than 150 mg/kg is virtually non-existent. Younger patients, male patients, and patients
with truncal acne derive maximum benefit from the higher dosages (1 mg/kg/day).
In these patients, dosages less than 0.5 mg/kg/day for a standard 4-month
course are associated with a high relapse rate. Treat older patients with
facial acne with a dosage of 0.5 mg/kg/day. Double the dosage if there is no
response at the end of 2 months. Subsets of patients
who are less likely to respond to isotretinoin and/or more likely to require
multiple or longer courses of treatment include adolescents under 16 years of
age who have nodulocystic acne, individuals with endocrine abnormalities, and
women with less severe acne. Hyperandrogenemia due to ovarian or adrenal
dysfunction should be excluded in women with a history of acne that is either
refractory to isotretinoin or has relapsed following appropriate courses of
isotretinoin. Scarred nodules and sinus tracts which represent sequelae from
previously active cystic acne do not respond to isotretinoin but may improve
with surgical modalities; the latter are generally delayed for at least 6–12
months after completing isotretinoin therapy to avoid the possible risk of
atypical healing or scarring responses.
Duration of therapy
A
standard course of isotretinoin therapy is 4-5 months. Approximately 85% of
patients are clear at the end of 4 months; 15% require longer treatment. Side
effects in all patients depend on the dosage. Treat for a longer duration at a
lower dosage if mucocutaneous side effects become troublesome.
Relapse and repeat courses of isotretinoin
Approximately
40 per cent of patients achieve long-term remission with a 120-mg cumulative
dose, 40 per cent require retreatment with topical therapy or oral antibiotics,
and 20 per cent require retreatment with isotretinoin, either for persistent
disease or for relapse. Relapse usually
occurs within the first 3 years after isotretinoin is stopped, most often
during the first 18 months after therapy. Some patients require multiple
courses of therapy. The response to repeat therapy is consistently successful
and safe, and side effects are similar to those of previous courses.
Isotretinoin therapy
Patients are seen
every 4 weeks. Isotretinoin is given in two divided doses daily. Many patients experience a moderate-to-severe
flare of acne during the initial weeks of treatment. This adverse reaction can
be minimized by starting at 10 to 20 mg twice each day and gradually increasing
the dosage during the first 4 to 6 weeks. Treatment is discontinued at the end of
16 to 20 weeks. Considering that improvement may continue for several months
after discontinuing isotretinoin, a hiatus of at least 2–3 months is
recommended before starting another course of therapy. Those with persistently
severe acne may receive a second course of treatment after the post treatment
observation period. Patients with moderate acne may respond to lower dosages
(0.3 mg per kg per day) and experience fewer adverse effects.
Response to therapy
At
dosages of 1 mg/kg/day, sebum production decreases to approximately 10% of pre-treatment
values and the sebaceous glands decrease in size. Maximum inhibition is reached
by the third or fourth week. Within a week, patients normally notice drying and
chapping of facial skin and skin oiliness disappears quickly. These effects
persist for an indefinite period when therapy is discontinued.
A lag period of 1–3 months may occur before the onset of the
therapeutic effect. During the first month, there is usually a reduction in
superficial lesions such as papules and pustules. New nodules evolve and
disappear quickly. A significant reduction in the number of nodules normally
takes at least 8 weeks. Facial lesions respond faster than trunk lesions.
Resistant patients
Younger
patients (14 to 19 years of age), male gender, and those who have severe acne
relapse more often. Truncal acne relapses more often than facial acne. A return
of the reduced sebum excretion rate to within 10% of the pre-treatment level is
a poor prognostic factor. Women whose acne does not clear after a total
cumulative dose of 150 mg/kg need laboratory and clinical evaluation of their
endocrinologic status. They may benefit from antiandrogen therapy.
Psychosocial implications
Patients
successfully treated with isotretinoin have significant reduction in anxiety
and depression. Patients with minimal
facial acne but with symptoms of dysmorphophobia (inappropriate depression
and/or anxiety response to mild acne) are often treated with long-term
antibiotic therapy with no perceived improvement. These patients respond to
isotretinoin in that they are satisfied with the cosmetic results achieved. The
incidence of relapse is greater than that of other acne patients and often
requires additional therapy in the form of antibiotics or further isotretinoin.
Laboratory Tests with
Isotretinoin
Required laboratory monitoring during therapy
includes a complete blood count, fasting lipid panel, and measurement of liver
transaminase levels.
|
Test |
Comments |
|
Pregnancy |
See iPLEDGE program guidelines* |
|
Triglyceride level† |
Performed during pre-treatment, after 2-3
weeks of treatment, and then at 4-week intervals. If levels exceed 350-400 mg/dl, repeat
measurement of blood lipids at 2- to 3-week intervals. Stop if value exceeds
700-800 mg/dl to reduce risk of pancreatitis. |
|
Complete blood cell count |
Performed before treatment and after 4-6
weeks of treatment. |
|
Liver function† |
Performed before treatment and after 4-6
weeks of treatment. |
Recommendations
from the European Directive on isotretinoin prescribing
|
Post
directive |
||
|
Dosage |
Start
0.5 mg/kg/day |
|
|
Indications
for use |
The
new recommendations suggest isotretinoin should only be used in severe acne
(nodular, conglobata) that has or is not responding to 3 months’ appropriate systemic
antibiotics and topical therapy; the inference of this being that it should
now not be used at all as first line therapy |
|
|
Age |
Not
indicated in children <12 years |
|
|
Monitoring |
Baseline
investigations : Liver enzymes and lipids should be checked before but at 1 month and 3 monthly
throughout the course of treatment |
Side effects of isotretinoin
The
most common adverse effects of isotretinoin involve the skin and mucous
membranes and are dose-dependent and are reversible shortly after discontinuing
treatment. Patients with side effects can be managed at a lower dosage for a
period long enough to reach the 120 mg/kg cumulative dose level. Explain to
patients that the long-term benefit is related to the cumulative dosage, not to
the duration of therapy.
Skin and mucous membrane adverse effects
Dose-dependent mucocutaneous toxicity is the most commonly
observed side effect of oral retinoids, and it reflects decreased production of
sebum, reduced stratum corneum thickness, and altered skin barrier function.
Dry lips or cheilitis is the earliest and the most frequent finding. Application
of emollients should be started with the initiation of therapy to minimize
drying. Dryness of the mouth (accompanied by thirst),
nasal mucosa (associated with fragility and epistaxis), and eyes are other
potential manifestations.
Xerosis
of the skin and associated pruritus, peeling (especially of the palms and
soles), and fissuring (particularly of the fingertips) are frequent side
effects. Exacerbations of atopic dermatitis may occur. Photosensitivity is
occasionally observed, in particular with isotretinoin, and probably reflects a
reduction in the thickness of the stratum corneum. Staphylococcus aureus colonization correlates with
isotretinoin-induced reduction in sebum production and may lead to overt
cutaneous infections. These patients may need treatment with an
intermediate‐strength
corticosteroid ointment combined with an oral antistaphylococcal therapy and/or
topical mupirocin 2% ointment. Routine use of moisturizers and infrequent
washing are recommended. Diffuse hair loss (telogen
effluvium) is a relatively common complaint, although objective alopecia tends
to occur only at high dosage levels. Effects on the nail apparatus can include
thinning, fragility, and shedding of the nail plate as well as paronychia-like
changes with periungual granulation tissue that can resemble pyogenic
granulomas.
With
the institution of isotretinoin therapy, induction of an acne fulminans-like
flare and excessive granulation tissue may occur at the sites of healing acne
lesions and is more likely to develop in patients who have pre-existing
crusted, draining, or ulcerated lesions. Granulation tissue can be controlled
with intralesional steroid injections or silver nitrate sticks. Cutaneous infections (in particular with Staphylococcus
aureus) can also occur.
Teratogenicity
Teratogenicity
is a serious potential complication. Fifty per cent of pregnancies
spontaneously abort, and of the remainder about half of the infants are born
with cardiovascular or skeletal deformities.
Female patients of childbearing potential must have at least one
negative pregnancy test before starting treatment and must practice effective
contraception for 1 month prior to, during, and for 1 month after completing
therapy. In the US, prescription of isotretinoin requires all physicians and patients
to register with a pregnancy risk management program (iPLEDGE™), which mandates
monthly office visits for all patients (with counselling not to share the
medication) and monthly pregnancy testing for female patients with childbearing
potential. Patients taking isotretinoin should not
donate blood while on therapy and for 1 month after the last dose.
Plasma lipid abnormalities
Hypertriglyceridemia
is the most frequently observed systemic effect of retinoid therapy.
Isotretinoin elevates triglycerides in 25–50% and cholesterol in 20–30% of
treated patients; however, severe elevations are uncommon and typically develop
within the first two months of therapy. A concomitant increase in total and
low-density lipoprotein (LDL) cholesterol is frequently observed. Overweight
subjects are 6 times more likely to develop significant elevations in serum
triglyceride levels, and subjects with elevated baseline triglyceride levels
are 4.3 times more likely to develop significant elevations. In cases of severe retinoid-induced hypertriglyceridemia,
eruptive xanthomas and acute hemorrhagic pancreatitis may occur.
Baseline
fasting serum lipid levels should be obtained before initiating isotretinoin
therapy and then monthly for the first 2 months and then at 3-month intervals
is adequate if baseline lipid levels are normal, there are no increases in
dosage, and risk factors (obesity, high alcohol intake, diabetes) are absent.
More recently, less frequent monitoring (e.g. only at baseline and after 2
months of treatment if normal) has been recommended for young healthy adults
receiving isotretinoin for acne. Discontinuation of therapy is suggested if
fasting triglycerides reach 800 mg/dl (8 g/l).
Ophthalmologic
side effects
The
most common ocular retinoid effects are dryness and irritation. Xerophthalmia
due to decreased meibomian gland secretions may prohibit the use of contact
lenses and can lead to blepharoconjunctivitis, keratitis, or corneal opacities.
Alterations in visual function, mainly nyctalopia (reduced night vision),
excessive glare sensitivity, and changes in colour perception, have also been
reported. Competitive inhibition of ocular retinol dehydrogenase by retinoids,
resulting in decreased rhodopsin formation, may be the cause of nyctalopia.
Central
nervous system and psychiatric effects
CNS
side effects are rare. Although individual signs of increased intracranial
pressure, such as headache, nausea and vomiting, are occasionally observed, the
complete pseudotumorcerebri syndrome with papilledema and blurred vision is
very rare. Concomitant use of other drugs associated with intracranial
hypertension (e.g. tetracyclines) is considered a risk factor for developing
pseudotumorcerebri and should therefore be avoided. Examination for papilledema
should be performed immediately when a patient receiving retinoid therapy
complains of a persistent headache, especially if it is accompanied by visual
changes, nausea or vomiting, or when pseudotumorcerebri is otherwise suspected.
Mood
changes including depression are common among adolescents acne patients treated
with isotretinoin. Patients with depression may actually benefit from
isotretinoin. Increased aggression has been identified in some male patients
and the FDA has advised clinicians to warn about this possible side effect. If
there is any doubt, the drug must be withdrawn. To date, no firmly established
causal association with depression or suicide attempts has been demonstrated.
Adverse
effects of isotretinoin: very common.
|
Type
of disorder |
Very
common (≥1/10) |
|
Blood
and lymphatic system |
·
Anaemia ·
Increased ESR ·
Thrombocytopenia ·
Thrombocytosis |
|
Eye |
·
Blepharitis ·
Conjunctivitis ·
Dry eyes ·
Eye irritation |
|
Hepatobiliary |
·
Increased transaminase |
|
Skin
and subcutaneous tissues |
·
Cheilitis ·
Dermatitis ·
Dry skin ·
Localized exfoliation ·
Pruritus ·
Erythematous ·
Skin fragility |
|
Musculoskeletal
and connective tissue |
·
Arthralgia ·
Myalgia ·
Back pain |
|
Investigation |
·
Increased triglycerides ·
Decreased high‐density lipoprotein |
Adverse effects of isotretinoin: common.
|
Type
of disorder |
Common
(≥1/100, <1/10) |
|
Blood
and lymphatic system |
·
Neutropenia |
|
Nervous
system |
·
Headache |
|
Respiratory,
thoracic and mediastinal |
·
Epistaxis ·
Nasal dryness ·
Nasopharyngitis |
|
Investigation |
·
Increased blood cholesterol ·
Increased blood glucose ·
Hematuria ·
Proteinuria |
Adverse effects of isotretinoin: rare.
|
Type
of disorder |
Rare
(≥1/10 000, <1/1000) |
|
Immune
system |
·
Allergic skin reaction ·
Anaphylactic reactions ·
Hypersensitivity |
|
Psychiatric |
·
Depression ·
Aggravated depression ·
Aggressive tendencies ·
Anxiety ·
Mood alterations |
|
Skin
and subcutaneous tissues |
·
Alopecia |
Adverse effects of isotretinoin: very rare.
|
Type
of disorder |
Very
rare (≥1/10 000) |
|
Infection |
·
Gram‐positive
(mucocutaneous) bacterial infection |
|
Blood
and lymphatic system |
·
Lymphadenopathy |
|
Metabolism |
·
Diabetes ·
Hyperuricaemia |
|
Psychiatric |
·
Abnormal behaviour ·
Psychotic disorder ·
Suicidal ideation ·
Suicide attempt ·
Suicide |
|
Nervous
system |
·
Benign intracranial hypertension ·
Convulsions ·
Drowsiness ·
Dizziness |
|
Eye |
·
Blurred vision ·
Cataract ·
Color blindness ·
Contact lens intolerance ·
Corneal opacity ·
Decreased night vision ·
Keratitis ·
Papilloedema ·
Photophobia ·
Visual disturbances |
|
Ear |
·
Impaired hearing |
|
Vascular |
·
Vasculitis (i.e. granulomatosis with
polyangiitis, allergic vasculitis) |
|
Gastrointestinal |
·
Colitis ·
Ileitis ·
Dry throat ·
Gastrointestinal hemorrhage ·
Hemorrhagic diarrhea ·
Inflammatory bowel disease ·
Nausea ·
Pancreatitis |
|
Hepatobiliary |
·
Hepatitis |
|
Skin
and subcutaneous tissues |
·
Acne fulminans ·
Aggravated acne (acne flare) ·
Erythema (facial) ·
Exanthema ·
Hair disorders ·
Hirsutism ·
Nail dystrophy ·
Paronychia ·
Photosensitivity reaction ·
Pyogenic granuloma ·
Skin hyperpigmentation ·
Increased swelling |
|
Musculo‐skeletal and connective tissue |
·
Arthritis ·
Calcinosis (calcification of ligaments and
tendons) ·
Premature epiphyseal fusion ·
Exostosis ·
Hyperostosis ·
Osteopenia ·
Tendonitis |
|
Renal
and urinary |
·
Glomerulonephritis |
|
General |
·
Increased formation of granulation tissue ·
Malaise |
|
Investigation |
·
Increased creatine phosphokinase |
Significant
systemic effects are uncommon; headaches may uncommonly be an early feature of
benign intracranial hypertension and arthralgia is seen most frequently in
those patients participating in regular and heavy exercise. Tetracyclines,
including doxycycline and minocycline, must not be prescribed with
isotretinoin, as both drugs may produce benign intracranial hypertension.
An
acute flare of acne early in a course of isotretinoin is a recognized problem
in about 6% of cases. If the acne is very inflammatory, a lower dose of
isotretinoin alongside oral corticosteroids may be required (e.g. 0.5–1.0
mg/kg/day for 2–3 weeks). Predisposing risk factors for a flare include the
presence of macrocomedones and nodules. If macrocomedones are present, light
cautery or hyfrecation should be done prior to starting the isotretinoin. If a
severe flare occurs, 0.5–1.0 mg/kg/day oral prednisolone is needed over a
period of 2–3 weeks followed by a tapering of dose the following 6 weeks. The
isotretinoin should either be stopped or reduced. If stopped, the drug can be
slowly reintroduced at a dose of 0.25 mg/kg/day, and then increased or
decreased as response dictates.
Reduced
efficacy has been noted when isotretinoin is taken with heavy alcohol intake.
Isotretinoin is metabolized by cytochrome P450 enzymes, inducible by ethanol
and inhibited by some drugs, for example ketoconazole. Hence, increased drug
levels of isotretinoin may occur if combined with imidazole fungistatics.
Salicylic acid and indometacin represent acidic drugs with a high affinity for
albumin. If present in the blood in high therapeutic concentrations, they may
displace isotretinoin from protein binding sites, resulting in an increase in
the unbound concentration of the drug. Carbamazepine plasma levels decrease
when concurrent isotretinoin is taken, hence careful monitoring should be
considered in epileptics on carbamazepine if requiring isotretinoin. Vitamin
supplements containing vitamin A should be avoided alongside isotretinoin, as
additive toxic effects could ensue.
Alternative Treatments for Acne Vulgaris
|
Treatment |
Comment |
|
Comedone extraction |
Performed with comedone extractor |
|
Injections |
Intralesional triamcinolone injected into
large cysts or nodules |
|
Light therapy |
Blue light (may photo inactivate P.
acnes) |
|
Red light (may have anti-inflammatory
effect) |
|
|
Combination blue-red light |
|
|
Intensed pulse light (IPL) |
|
|
Photodynamic therapy (PDT) |
|
|
Laser therapy |
KTP, pulsed dye laser (rarely used) |
|
Resurfacing laser (including both
nonablative and ablative resurfacing lasers); useful for acne scarring |
|
|
Dermabrasion/dermasanding |
Useful for acne scarring |
|
Collagen injection |
Useful for acne scarring |
|
Chemical peels |
Useful for acne scarring and
hyperpigmentation |
|
Punch grafts/tissue augmentation |
Useful for acne scarring |
|
Trichloroacetic acid |
Useful for atrophic acne scars |
|
Radiation therapy |
Outdated modality |
|
|
|
Surgical
Treatment
Light
electrocautery or hyfrecation has been shown to help patients with multiple macrocomedones;
these are usually whiteheads but occasionally blackheads (up to 1.5 mm
diameter), and chloracne can be improved. A topical anaesthetic preparation is
applied beneath an occlusive dressing. The cautery or hyfrecation should be set
as low as possible to produce little or no pain. The aim is to produce very low‐grade
thermal damage. The treatment of each lesion takes seconds and is associated
with very little scarring or post‐inflammatory
pigmentation. This therapy is more effective than topical tretinoin for
macrocomedones.
Comedo
extraction can improve the cosmetic appearance of acne and aid in therapeutic
responsiveness to topical comedolytic agents. The keratinous contents of open
comedones may be expressed using a comedo extractor. Nicking the surface of a
closed comedo with an 18-gauge needle or a #11 blade allows easier expression.
Extraction is especially beneficial for deep, inspissated and persistent
comedones. This procedure should be used in conjunction with a topical retinoid
or other comedolytic treatment for maximum benefit. Comedo extraction should
not be performed on inflamed comedones or pustules because of the risk of
scarring. In selected patients, cryotherapy represents another surgical option
for the treatment of comedonal acne.
Intralesional
injection of corticosteroid (triamcinolone acetonide 2–5 mg/ml) can quickly
improve the appearance and tenderness of deep, inflamed nodules and cysts.
Larger cysts may require incision and drainage prior to injection. The maximal
amount of corticosteroid used per lesion should not exceed 0.1 ml. The risks of
corticosteroid injections include hypopigmentation (particularly in darkly
pigmented skin), atrophy, telangiectasias, and and
yellow–white dermal deposits of the medication.
Laser and light therapies
Light and laser
therapies can be used for the treatment of acne. Examples include visible
light, pulsed-dye laser, and photodynamic therapies.
Photodynamic
therapy utilizing topical 5-aminolevulinic acid together with various light
sources (e.g. blue, red, intense pulsed) or lasers (e.g. pulsed dye, 635 nm red
diode) as well as methyl aminolevulinate plus red light have been successfully
used to treat acne. In addition, blue or intense pulsed light alone and lasers
such as the pulsed dye, the 1320 nm neodymium: YAG and especially the 1450 nm
diode may be of therapeutic benefit for inflammatory acne.
Chemical peels
Low-concentration chemical peels are also beneficial for the reduction of comedones. The α-hydroxy acids (including glycolic acid), salicylic acid and trichloroacetic acid are the most common peeling agents. These lipid-soluble comedolytic agents act by decreasing corneocyte cohesion at the follicular opening and assist in comedo plug extrusion. Such agents are generally well tolerated by most skin colors and types, and they can be used by the patient at home or in the dermatologist’s office. Higher-concentration glycolic acid peels (20–70%, depending on the patient’s skin type) and the less predictable phenol peel may also be performed in the office setting. Risks of chemical peels include irritation, pigmentary alteration and scarring. Many dermatologists worldwide use light chemical peels with the aim of helping to remove comedones as well as superficial scarring and hyper pigmentation.
One
of the most distressing consequences of acne vulgaris is scarring. Surgical
treatments should be aimed at the type of scarring present. Laser resurfacing
(fractional as well as traditional), dermabrasion and deeper chemical peels
seek to reduce the variability of the skin surface and smooth out depressed
scars that improve when the skin is stretched. For discrete depressed scars,
soft tissue augmentation can be temporarily beneficial. Filler substances used
include poly-L-lactic acid, calcium hydroxylapatite and autologous fat. Punch
grafting is an option for patients with “ice-pick” scarring. Surgical
subscision is also a commonly used technique in the management of acne scars.
For larger hypertrophic scars, aggregated pitted scars and sinus tracts,
full-thickness surgical excision may result in improved scar placement and a
better cosmetic appearance.
Algorithm of therapeutic options for
neonatal, infantile, mid‐childhood and prepubertal acne
|
Acne category |
Treatment options |
|
Neonatal |
Gentle cleaners, oil‐free emollients If marked pustules
topical azole cream |
|
Infantile Prepubertal |
First line Benzoyl peroxide or
topical retinoid (if primarily comedonal) Fixed combination
products if mixed lesions all indicated from 12 years with the exception of
0.1% adapalene/2.5% BPO which is indicated from 9 years Second line for more severe
disease Oral erythromycin
(oral trimethoprim if allergic to macrolides) combined with benzoyl peroxide
to avoid emergence of antibiotic‐resistant P. acnes ± topical retinoid Third line Severe recalcitrant
scarring acne, exclude underlying hyperandrogenism Consider oral
isotretinoin |
|
Mid‐childhood |
Exclude
underlying pathology and treat as infantile and prepubertal |
Treatment of Acne in Pregnancy
ABFM 2016
In women who are planning pregnancy or who is pregnant, acne
can be particularly bothersome given the physiologic changes as well as the
unpredictable nature of acne during this time. Acne often improves during
the first trimester but may worsen during the third trimester as a result of
increased maternal androgen concentrations and the resultant effects on sebum
production. In addition to hormonal changes, pregnancy-associated
immunologic factors may also contribute. Inflammatory lesions tend to be
more common than noninflammatory lesions, often with involvement extended to
the trunk. Patients with a history of acne are more prone to developing acne
during pregnancy.
Management
of acne in pregnant patients can be challenging because many widely used and
effective therapeutic options are contraindicated or not recommended. For mild
acne characterized primarily by non-inflammatory lesions, topical azelaic acid
or benzoyl peroxide can be recommended as baseline therapy. For acne involving
inflammatory lesions, starting with a combination of topical erythromycin or
clindamycin with benzoyl peroxide is recommended. Moderate to severe
inflammatory acne can be managed with oral erythromycin or cephalexin, which is
safe when used for only a few weeks. A course of oral prednisolone no longer
than a month may be useful for treating fulminant nodular cystic acne after the
first trimester. In general, topical and oral antibiotics should not be used as
monotherapy, but should be combined with topical benzoyl peroxide to decrease
bacterial resistance. Oral
retinoids are teratogenic and absolutely contraindicated for women who are
pregnant or considering pregnancy. The risk-to-benefit ratio, efficacy,
acceptability, and costs are considerations when choosing a treatment for acne
in pregnancy.
Topical Treatments
For mild to moderate
acne, topical therapy is the standard of care. It is also an important
component of the regimen for more severe acne and acts synergistically with
oral agents. Quantifiable systemic absorption of topical anti-acne agents must
be considered in pregnancy.
Azelaic Acid (20% Cream)
Azelaic acid is classified as pregnancy category B. Azelaic
acid is a naturally occurring dicarboxylic acid with antimicrobial,
comedolytic, and mild anti-inflammatory properties, with an added benefit of
decreasing post-inflammatory hyper pigmentation (Antityrosinase
activity). There are no indications that Propionibacterium
acnes may become resistant to azelaic acid. Following topical
application, approximately 4% of the drug is absorbed systemically.
Benzoyl Peroxide
Benzoyl peroxide is classified as pregnancy category C.
Approximately 5% is absorbed systemically, and it is completely metabolized
into benzoic acid, a food additive. Because of rapid renal clearance, no
systemic toxicity is expected, and the risk of congenital malformations is
theoretically small. Benzoyl peroxide is available as both prescription
and nonprescription products in a variety of concentrations and vehicles. It
has antimicrobial, comedolytic, and anti-inflammatory properties. To date, resistance
of P. acnes to benzoyl peroxide has not been
identified. Benzoyl peroxide is considered safe during pregnancy and helps
to prevent the development of resistance when used in conjunction with
antibiotics.
Topical Antibiotics
Topical antibiotics have long been used for the treatment of
inflammatory acne; erythromycin and clindamycin are the 2 most commonly
prescribed agents. Both are classified as pregnancy category B. Short-term use
of topical erythromycin and clindamycin is safe during pregnancy. However,
studies addressing the effects of chronic use are not available. Given the
reported association of cases of Clostridium difficile diarrhea
with topical clindamycin, it should be used with caution in patients with a
history of gastrointestinal disease. Topical clindamycin and erythromycin
reduce the amount of P. acnes in the sebaceous follicle
by inhibiting bacterial protein synthesis and thereby suppressing inflammatory
acne. Combining topical antibiotic therapy with topical benzoyl peroxide
decreases the development of bacterial resistance and improves treatment
efficacy.
Oral Antibiotics
Oral antibiotics improve inflammatory acne by inhibiting the
growth of P. acnes in the pilosebaceous unit. Tetracycline
antibiotics (including doxycycline and minocycline) also exert direct
anti-inflammatory effects. The agents most commonly used by patients who are
not pregnant include doxycycline, minocycline, erythromycin, azithromycin,
cephalexin, and trimethoprim-sulfamethoxazole. Because of increasing bacterial resistance,
it is generally recommended to (1) combine topical benzoyl peroxide with oral
antibiotics, (2) limit the use of oral antibiotics to as short duration as
possible, and (3) avoid oral antibiotics for acne maintenance
therapy. Switching between different oral antibiotics should also be
avoided when possible to limit the development of bacterial resistance; if 1
oral antibiotic has proven effective in the past, it should be prescribed
again. Oral antibiotics should be prescribed during pregnancy only when
need has been clearly established.
Erythromycin (250–500
mg, 2–4 times/day) is a macrolide
in pregnancy category B. Single doses of the drug cross the placenta poorly,
resulting in low concentrations in fetal tissue. Erythromycin is generally
considered safe during any stage of pregnancy when administered for a few
weeks. It may be considered the antibiotic of choice for treatment of
severe inflammatory acne in pregnant women. However, long-term use of the drug
(>6 weeks) has not been studied. Notably, erythromycin estolate is
contraindicated because of drug-related maternal hepatotoxicity.
Azithromycin
(250
mg 3 times in a week) is
another macrolide that is classified in FDA pregnancy category B. Azithromycin
is considered compatible with pregnant patients with acne but has less
available safety data than erythromycin.
Cephalexin
(500
mg twice daily) is a
first-generation cephalosporin with anti-inflammatory properties and is
considered a pregnancy category B drug. While effective as an anti-acne agent,
there is some concern about the development of resistance against Staphylococcus.
It
is important to note that additional evidence is needed regarding the
recommended durations of these therapies. The effects of chronic usage of these
antibiotics on the fetus are not known. This consideration must be weighed
against the severity of acne and alternative topical therapies. Use of systemic
antibiotics should be restricted to the second and third trimesters, after the
completion of organogenesis, with duration of therapy limited to 4 to 6 weeks.
Oral Corticosteroids
Severe acne that is resistant to antibiotic therapy may
benefit from the use of oral corticosteroids. Prednisone belongs to FDA
pregnancy category C. Human studies showed an increased risk of oral cleft and
a slight increase in miscarriage rates and preterm births. Few data are
available on the transfer of intralesional or topical steroids across the
placenta; although it has been shown that topical steroids can be absorbed
systemically. Prednisone may be used for severe or fulminant acne cases
after the first trimester. Conservative use of steroids, such as small amounts
of intralesional steroids and short courses of oral steroids required for rare,
fulminant cases of acne vulgaris, is unlikely to pose additional risks to the
fetus. Prednisone dosage should be limited to <20 mg/day over a course
of no more than 1 month during the third trimester.
Treatment Algorithm for Acne in Pregnancy
|
Type of Acne |
Treatment |
FDA
Pregnancy Drug Class |
Evidence
Rating |
|
Noninflammatory |
|||
|
Comedonal |
Azelaic acid |
B |
Likely to be beneficial |
|
Inflammatory |
|||
|
Mild to moderate |
Azelaic acid + |
B |
Likely to be beneficial |
|
Benzoyl peroxide or |
C |
Beneficial |
|
|
Topical erythromycin or |
B |
Beneficial |
|
|
Topical clindamycin + |
B |
Beneficial |
|
|
Benzoyl peroxide |
C |
Beneficial |
|
|
Moderate to severe |
Oral erythromycin or |
B |
Likely to be beneficial |
|
Oral cephalexin + |
B |
||
|
Benzoyl peroxide with or without |
C |
Beneficial |
|
|
Azelaic acid or |
B |
Likely to be beneficial |
|
|
Intralesional steroid injections |
C |
||
|
Fulminant |
Oral erythromycin + |
B |
Likely to be beneficial |
|
Benzoyl peroxide + |
C |
Beneficial |
|
|
Azelaic acid + |
B |
Likely to be beneficial |
|
|
Oral prednisone(short-term) |
C |