Hidradenitis
suppurativa
Salient
features
·
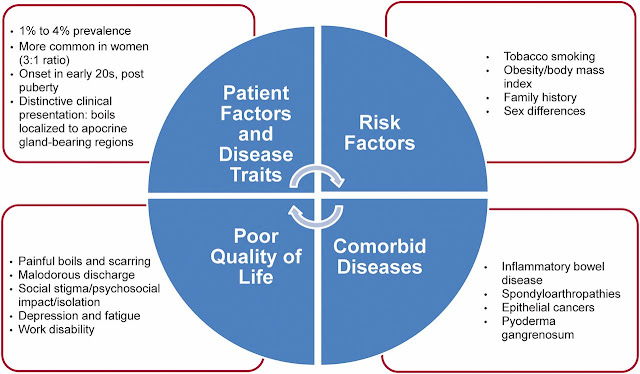
Hidradenitis
suppurativa is a chronic and debilitating inflammatory disorder of the hair
follicles with an underlying immune system imbalance that affects genetically
predisposed individuals and that localizes to intertriginous and anogenital
regions of the body. The course of disease can be modified by exogenous
triggers or aggravating factors.
·
Lesions
are characterized by inflammatory nodules, subcutaneous abscesses, and sinus
tracts.
·
Reproductive-age
women are disproportionately affected.
·
Hyperkeratotic
plugging of the terminal hair follicle is a consistent histologic finding of
early disease and is thought to be the primary pathophysiologic event.
Introduction
The
first International Hidradenitis Suppurativa (HS) Research Symposium (2006,
Dessau, Germany) formulated the following definition: HS is a chronic, inflammatory, recurrent, debilitating, skin disease that usually presents after pubertywith painful, deep‐seated inflamed lesions, primarily within the folded area of
the skin that contain both terminal hairs and apocrine glands. The disease
primarily affects terminal hair follicle. Approximately one‐third of patients have a family member with HS.
Epidemiology
Age
HS typically starts at or soon after
puberty; the average age of onset is between second and third decade, with a
sharp decline after the fifth decade.
Sex
Women are affected three times as
often as men; estimated
to affect 4% of the female population. Topographical
distribution of lesions can vary between sexes. For example, perianal and gluteal
disease are more common in males, whereas inguinal and submammary disease are
more common in females. The most commonly affected site is axilla.
Associated
diseases
Diseases associated with HS include
disorders of the follicular occlusion tetrad, systemic inflammatory disorders
and genodermatoses.
Follicular
occlusion tetrad
Acne conglobata, dissecting
cellulitis of the scalp and pilonidal sinus can coexist with HS; together they
comprise the ‘follicular occlusion tetrad’.
Inflammatory
disorders
The
coexistence of HS and Crohn disease, particularly with perianal involvement,
has been associated with a more fulminant course. Perianal Crohn disease may be
clinically indistinguishable from perianal HS. Other
associated inflammatory disorders include pyoderma gangrenosum and the
syndromes SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis), PAPA
(pyogenic arthritis, pyoderma gangrenosum and acne), PASH (pyoderma gangrenosum,
acne conglobata and suppurative hidradenitis) and PAPASH (pyogenic arthritis,
pyoderma gangrenosum, acne and suppurative hidradenitis).
Genodermatoses
Genodermatoses associated with HS or
HS‐like lesions include keratosis ichthyosis deafness syndrome,
pachyonychia congenita, steatocystoma multiplex and Dowling–Degos disease.
Most of these diseases belong to the group of auto inflammatory
disorders, where Th17 cell cytokines seem to play a central role.
Pathophysiology
Proposed Pathogenesis
Recent studies propose the following
mechanism:
1.
The process starts with the
infiltration of lymphocytes around the terminal hair follicle
(Perifolliculitis)
2.
Perifolliculitis may lead to
infundibular hyperkeratinisation and subsequent blockage by keratin plugging.
3.
Dilatation of the hair follicle,
followed by its rupture, leaking its contents, including keratin, bacteria,sebum
and hairs into the surrounding dermis. This incites a vigorous
chemotactic response and abscess formation
with the formation of painful, deep dermal abscesses and apocrinitis as
the inflammation spreads. The deep part of the follicle appears to be involved.
4.
The presence of secondary bacterial infection
of inflamed
hair follicles further promotes the infiltration of
immune cells and inflammation, leading to the formation of pus. Epithelial
strands are generated, possibly from ruptured follicular epithelia, and form
sinus tracts with subsequent extensive scarring. Common secondary bacterial
infections are staph aureus, streptococcus pyogens and gram negative
organinsms.
Predisposing
factors
Obesity and smoking
Obesity and smoking are the two main
exacerbating
factors associated with HS. Obesity is often
regarded as an exacerbating factor by increasing shearing forces, occlusion,
keratinocyte hydration, and maceration and also
increased pro‐inflammatory cytokine release from visceral fat at intertriginous skin sites.
Obesity
may also exacerbate disease by creating a state of androgen excess. There is an increased prevalence of smoking amongst patients
with HS. It
is postulated that smoking affects polymorphonuclear cell chemotaxis. There is
a strong association with current smoking. Smoking cessation may improve the
clinical course of the disease.
Hormones and Androgens
The
tendency of HS to develop at puberty or post puberty suggests an androgen
influence. Hormonal influences are supported by
a female preponderance, improvement during pregnancy and disease flares during
postpartum, in association with the oral contraception pill, and in the
premenstrual period (approximately 50% of patients). Antiandrogen therapy has
also demonstrated therapeutic benefit in some studies. Clinical signs of virilization are, however, usually absent
and circulating androgen levels are typically normal. Additionally, unlike
the sebaceous glands, the apocrine glands are not affected by androgens. Thus,
the influence of androgens on HS is unclear.
Host defense
Alterations of the innate immune
system are thought to underlie disease pathogenesis. Overproduction
of both IL-1β and tumor necrosis factor
(TNF)-α has been observed lesional skin,
suggesting the involvement of the innate immune system as well. In addition, a
therapeutic response to TNF-α inhibitors and
to IL-1 receptor antagonists has been noted in some studies. Increased serum
levels of IL-2, which correlate with disease activity, have also been detected,
as well as increased expression of IL-12, -17, and -23 within lesional skin.
Lastly, high copy numbers of the beta-defensin cluster are noted to confer
genetic susceptibility to hidradenitis suppurativa.
Pathology
There is a heavy mixed inflammatory
cell infiltrate including histiocytes and giant cells in the lower half of the dermis
that extends to interfollicular apocrine and eccrine structures and deep into
the subcutis. Abscesses are present in active cases, and they may connect to
the skin surface via a sinus tract. The sinus tracts contain inflammatory cells
and keratinous debris. Granulation tissue with inflammatory and occasional foreign body
giant cells is present in up to 25% of biopsies. In
chronic disease, there may be extensive fibrosis with destruction of
pilosebaceous follicles and eccrine and apocrine sweat glands.
Diagnostic criteria
All three diagnostic criteria must
be met for a diagnosis of HS to be made.
1.
Typical lesions that are deep‐seated, painful nodules: ‘blind boils’ in early primary
lesions; abscesses, draining sinus tracts, bridged scars and paired or
multiheaded open pseudocomedones in secondary lesions.
2.
Typical topography: axillae, groin,
perineal and perianal region, buttocks and infra‐
and intermammary folds.
3.
Chronicity and recurrence of
lesions.
Clinical
features
It is a chronic condition characterized by recurrent “boils”
and draining sinus tracts with subsequent scarring. Initially,
inflammatory nodules and sterile abscesses develop in the flexural areas. These
lesions may be very tender and extremely painful. Over time, sinus tracts and
scars may develop. This is accompanied by chronic drainage of malodorous
discharge, leading to a marked degree of frustration, embarrassment, self-consciousness
and depression. The discharged fluid is often a
mixture of serous exudate, blood and pus, in varying proportions. Scarring is typically bridged or ‘rope‐like’, it can be hypertrophic or atrophic, producing depressions
especially on the buttocks, and may be associated with contractures. Pseudo‐ (secondary) comedones are often seen, typically paired,
polyporous and grouped. Lesions are localized to inverse (flexural) areas. The
commonest sites are the axillae and inguinal and ano‐genital regions, including the external genitalia and the
perineal, perianal and gluteal skin. Sub‐
and intermammary skin can also be affected, as can, less commonly,
retroauricular, preauricular and occipital skin. The lesions are often bilateral.
Classification
of severity
The Hurley staging system refers to three stages based on
the presence and extent of sinus tracts and scarring.
|
Hurley staging system |
|
|
1.
Stage I – One
or more recurrent abscess formation with no sinus tract or scar formation 2.
Stage II –
One or more widely separated recurrent abscesses, with sinus tract and scar
formation 3.
Stage III –
Multiple interconnected abscesses, sinus tracts and scarring diffusely
involving an entire region |
|
Complications
and co‐morbidities
Secondary bacterial infection should
be suspected when flares are preceded by smarting pain or associated with the
development of pustules. Anal,
urethral, or rectal strictures may develop from chronic inflammation. Fistula formation to the gastrointestinal tract (anal canal
and rectum), genito‐urinary tract (urethra, bladder and vagina) and peritoneum
are extremely rarely described, and when seen should trigger examination for
Crohn disease. Additionally,
disfiguring persistent penile, scrotal, or vulvar lymphedema due to blockade or
destruction of local lymph drainage routes subsequent to chronic and recurrent
inflammation may develop, giving rise to significant functional impairment.
Once this complication appears, no medical treatment is effective and surgical
reconstruction may be necessary. Squamous cell carcinoma (SCC) may rarely
develop in chronically inflamed and scarred areas in individuals with
long-standing disease. Malignant transformation occurs most commonly on the gluteal skin of male patients, and
carries a poor prognosis.
Disease
course and prognosis
Chronicity is the hallmark. The mean
duration is 18.8 years. Milder forms (Hurley stage I) are more frequent and
affect approximately two‐thirds of patients, with intermediate disease (Hurley stage
II) affecting one‐quarter and severe disease (Hurley stage III) about one‐fifth of patients. In patients older than 50 years, spontaneous
remission may occur over time.
Hidradenitis suppurativa – grading systems and therapeutic
ladder. Additional scoring systems are used in clinical trials. In the
Revuz modification of the Sartorius grading system, five regions (axilla,
breast, inguino-femoral, perianal, perineal) are scored, with additional
modifications including the addition of abscesses to fistulae. Both
Hidradenitis Suppurativa Clinical Response (HiSCR) and a Physician’s Global
Assessment (PGA) Scale have been utilized as has a refinement of the Hurley
staging system in which stages I and II are subdivided into A,B,C subtypes.
|
HIDRADENITIS SUPPURATIVA –
GRADING SYSTEMS AND THERAPEUTIC LADDER |
|
|
Hurley staging system |
|
|
.
Stage
I – one or more abscesses with no sinus tract or scar formation .
.
Stage
II – one or more widely separated recurrent abscesses, with sinus tract and
scar formation .
.
Stage
III – multiple interconnected sinus tracts and abscesses throughout an
affected region; more extensive scarring |
|
|
Sartorius grading system |
|
|
·
Anatomical
regions involved: axilla (left +/or right), groin (left +/or right), gluteal
(left +/or right) or other region (e.g. inframammary): 3 points per region
involved ·
Number
and scores of lesions for each region: nodules = 1; fistulae = 6 ·
The
longest distance between two relevant lesions*, i.e. nodules and fistulae, in each
region: <5 cm = 1; 5–10 cm = 3; >10 cm = 9 ·
Are
all lesions clearly separated by normal skin? In each region – yes 0/no
(Hurley III) 9 |
|
|
Therapeutic ladder |
|
|
Indication |
Therapeutic interventions |
|
General measures |
·
If
obese or overweight, weight reduction ·
Reduce
friction and moisture via loose undergarments, absorbent powders, and topical
aluminum chloride ·
Antiseptic
soaps ·
Smoking
cessation |
|
Hurley Stage I |
·
Intralesional
triamcinolone (5 mg/ml) injections into early inflammatory lesions ·
Topical
clindamycin ·
Eradication
of S. aureus carriage with topical mupirocin in
nose, axillae, umbilicus, and perianal regions ·
Oral
antibiotics tailored to results of bacterial cultures from pustular discharge
or abscess contents ·
Oral
antibiotic therapy (alone or in combination) for its anti-inflammatory effect
(rifampin + clindamycin, tetracycline, doxycycline, minocycline, dapsone,
trimethoprim–sulfamethoxazole) ·
Oral
anti-androgen therapy (e.g. finasteride) |
|
Hurley Stage II |
·
Oral
antibiotic therapy (see Stage I) ·
Acitretin ·
Systemic
immunosuppressive agents including adalimumab^, infliximab,
and cyclosporine Surgical treatments† ·
Limited
local excisions with second intention healing ·
CO2 laser ablation with second intention healing ·
Nd:YAG
laser treatments, at least 3–4 monthly sessions |
|
Hurley Stage III |
Medical treatments outlined for Stages I
and II Surgical treatments† ·
Early
wide surgical excision of involved areas ·
CO2 laser ablation with second intention healing |
* Or size if only one lesion.
^FDA- approved dosing
regimen: 160 mg (four 40 mg injections) on day 1 –or- 80 mg daily on days 1 and
2 followed by 80 mg on day 15 then 40 mg
on day 29 and weekly thereafter
† Incision and drainage is discouraged
given high rate of recurrence.
Adjuvant
treatment
1.
Weight reduction (if overweight) and
smoking cessation
2.
Reduce friction and moisture
(loose-fitting clothing and undergarments, absorbent powders, topical aluminum
chloride)
Analgesics
HS is painful and patients should be
offered appropriate analgesic therapy, including non‐steroidal anti‐inflammatory
therapy and paracetamol.
Topical
therapy
Antiseptic soaps and topical antibiotics (e.g. clindamycin
lotion 0.1% may reduce Staphylococcus aureus colonization and secondary
infection). Intranasal mupirocin (5-day course for nasal carriers of S. aureus).
Systemic
antibiotics
Combined treatment with clindamycin 300 mg b.d. and
rifampicin 300 mg b.d. given for 10 weeks resulted in remissions of up to 1 to 4 years regardless
of disease severity (Hurley stage I, II, or III). The
combination is well tolerated, as the most common adverse effects are
gastrointestinal discomfort and diarrhea (generally mild).
Other antibiotics
used to treat HS are doxycycline, minocycline, and rifampicin associated with
moxifloxacin and/or metronidazole, with variable response.
Anti‐inflammatory treatment
For
isolated number of tender lesions,
intralesional triamcinolone (3–5 mg) often ameliorates symptoms rapidly. For
more severe disease, short‐term systemic prednisolone (0.5–1.0
mg/kg body weight) or ciclosporin (3–5 mg/kg body weight), or longer term
treatment using dapsone (100 mg daily), have all been reported to be useful for
disease control.
Biological
agents
Tumour necrosis factor‐α antibodies appear to have a beneficial effect in moderate
to severe HS. The
most effective tumor necrosis factor α (TNF-α) blocker in HS is adalimumab. Adalimumab is considered the most specific
treatment for HS. Based on the data available, it is currently the main
drug for the treatment of refractory Hurley stage II disease or moderate to
severe Hurley stage III disease.
Adalimumab (a loading dose of 160mg
at week 0 and 80mg at week 2, followed at week 4 by 40mg every week, for a
total of 12 weeks).
Physical
intervention
Surgical removal of
all involved tissue, beyond clinically involved margins, is an effective
treatment modality.
Surgery is indicated
for the treatment of nodules and isolated fistulas and for severe, extensive
disease that does not respond to medical treatment. The choice of surgery and
size of margins are determined by the area affected and the degree of
involvement.
Several
surgical techniques are indicated for HS:
1.
Incision and drainage
2.
Unroofing and marsupialization
3.
Localized excision
4.
Wide excision
Incision and Drainage
Incision
with drainage is a simple technique that can be performed under local
anesthesia on an outpatient basis. It tends to result in rapid relief of pain
in the case of isolated nodules, but recurrence is common.
Punch debridement has also been proposed as a modification of this technique. This procedure involves centering a biopsy punch with a diameter of 5 to 7mm over an inflamed pilosebaceous unit, which is then debrided by digital pressure followed by curettage. The goal is to remove the remains of the sebaceous gland and/or the follicle containing cells involved in the generation of fistulas and fibrous tracts. Preliminary data suggest that recurrences are relatively infrequent with this technique.
Deroofing
Unroofing (or deroofing) with marsupialization is a simple technique that can also be performed on an outpatient basis.
Deroofing is a tissue‐saving technique, whereby the ‘roof’ of an abscess or sinus
tract is surgically removed either through electrosurgery (using a loop) or
conventional surgery. The ensuing defect is left open to heal by secondary
intention.
Unroofing is suitable
for recurrent painful stage I or II lesions, and results in acceptable cosmetic
results. Approximately 17% of lesions treated using this technique has been
found to recur within a mean of 4 to 6 months.
Localized surgery
Patients with few, clinically
stable, non‐inflamed lesions (nodules or sinus tracts) are most suitable
for localized surgery. Generally, complete surgical removal of the lesion is
required, suggesting that wider excisions have a better result than more
limited excision.
Extensive
surgery
In severe disease when entire sites
are involved with multiple interconnecting sinus tracts, the only curative
method is excision of the entire area involved.
Wide
excision involves removing an entire affected area with margins extending
beyond the visibly affected region. When used in combination with medical
measures and treatments, wide excision is the technique that is most likely to
achieve disease control in patients with chronic, extensive stage III disease.
The surgical defect can be reconstructed using simple local or free flaps, skin
grafts, tissue expanders, or simply closure by secondary intention.
Lasers and Light
CO2 laser evaporation
provides a method whereby all visibly affected tissue can be vaporized (i.e.
evaporating abnormal tissue under visual guidance until healthy tissue is
reached everywhere). The technique offers radical treatment whilst still being
tissue‐sparing. Postsurgical defects are usually left to heal by
secondary intention. Patient satisfaction with the technique is high.
Hair
removal lasers and intense-pulsed light systems also result in clinical
improvement by reducing the number of hair follicles and associated
inflammation. Long-pulsed (1064nm) Nd:YAG 1064 laser therapy has also been
described as effective for the treatment of Hurley stage II and III disease.
Radiotherapy
In selected patients with
particularly recalcitrant disease, radiotherapy may be considered.
PSYCHOLOGICAL MANAGEMENT
Patients
become very depressed because of pain, soiling of clothing by draining pus,
odor and the site of occurrence (anogenital area). Therefore, every effort
should be made to deal with the disease, using every modality possible.
Approach
to the treatment of hidradenitis suppurativa, based on the European guidelines
for hidradenitis suppurativa
|
Therapy |
Category
of Evidence |
Strength
of Recommendation |
|
1st Line |
||
|
Clindamycin (topical) |
IIb |
Possible
B |
|
Clindamycin/Rifampicin
(oral) |
III |
C |
|
Adalimumab (subcutaneous) |
Ib |
A |
|
Tetracycline (oral) |
IIb |
B |
|
Surgery |
||
|
Excision or Curettage of
Individual Lesions |
III |
C |
|
Total Excision of the Lesions and
Surrounding Hair-Bearing Skin |
IIb |
B |
|
Second Intention Healing |
IIb |
B |
|
Primary Closure |
III |
C |
|
Reconstruction with Skin Grafting
& NPWT |
III |
C |
|
Reconstruction with Flap Plasty |
Ia/IIa |
A/B |
|
Deroofing |
IV |
D |
|
Carbon Dioxide Laser Therapy |
Ib |
A |
|
Nd:YAG Laser |
Ib |
A |
|
IPL |
IV |
D |
|
2nd Line |
||
|
Zinc Gluconate
|
III |
C |
|
Resorcinol |
III |
C |
|
Intralesional Corticosteroids |
IV |
D |
|
Systemic Corticosteroids |
IV |
D |
|
Infliximab |
Ib/IIa |
B |
|
Acitretin/Etretinate |
III |
C |
|
3rd Line |
||
|
Colchicine |
IV |
D |
|
Botulinum Toxin |
IV |
D |
|
Isotretinoin |
IV |
D |
|
Dapsone |
IV |
D |
|
Cyclosporine |
IV |
D |
|
Hormones |
IV |
D |
|
Pain Control |
||
|
NSAIDS |
IV |
D |
|
Opiates |
IV |
D |
|
Dressings |
||
|
No studies have been published to
date on the use of specific dressing or wound care methodology in HS. Choice
of dressing is based on clinical experience. |
IV |
D |