Seborrheic dermatitis
Salient
features
- Seborrheic dermatitis is a common inflammatory skin disease affecting various age groups.
- Infantile and adult forms
- Erythematous, greasy, scaling patches and plaques appear on scalp, face, ears, chest, and intertriginous areas.
- Severe forms, like generalized erythroderma, rarely occur.
- Etiology is unclear but may be related to abnormal immune mechanism, active sebaceous glands, abnormal sebum composition, Malassezia (Pityrosporum) spp. and individual susceptibility.
- Can be a cutaneous sign of HIV infection
- Treatment is based on symptomatic control.
Introduction
Seborrheic dermatitis is a
common mild chronic eczema typically confined to skin regions with high sebum
production and the large body folds. Although its pathogenesis is not fully
elucidated, there is a link to sebum overproduction (seborrhea) and the
commensal yeast Malassezia.
Epidemiology
The
incidence of SD 2 to 5% of the general population and
notably peaks in three age groups, in infancy between 2 weeks and
12 months of age, during adolescence, and between age 30 and 60 years
during adulthood. This observation, together with the fact that SD occurs
only in seborrhoeic areas, already raise the question whether these incidence
peaks correlate with defined environmental, microbial and/or hormonal (eg
androgen) changes in the skin milieu.
Men are afflicted more often than women in all ages. Extensive
and therapy-resistant seborrheic dermatitis is an important cutaneous sign of
HIV infection.
Etiology and pathogenesis
Etiologic links with active sebaceous glands, abnormal sebum
composition, and Malassezia furfur (Pityrosporum ovale). The cause of seborrhoeic dermatitis is
not completely understood. It is associated with proliferation of various
species of the skin commensal malassezia, in its yeast
(non-pathogenic) form. The inflammation seen in seborrheic
dermatitis may be irritant, caused by toxic metabolites (such as the
fatty acids oleic acid, malssezin, and indole-3-carbaldehyde), lipase, and reactive oxygen species..
WORKING HYPOTHESIS
In contrast to the
conventional Malassezia‐centric view of SD
etiology, the working hypothesis is that intrinsic factors of the host—such as defective epidermal barrier (①) and/or changes in the amount or
composition of sebum (②)—may
be the root cause of seborrhoeic dermatitis (SD). These
changes can be brought about, for example by genetic predisposition, host
immune function, neuroendocrine factors, nutrition, medication and
environmental factors. Once these changes have occurred, they may provide favorable
conditions for the commensal Malassezia to over colonize the area and become the dominant
species, alter skin microbiota (③), and for yeast metabolites such
as oleic acid to penetrate the defective barrier and elicit a rather non‐specific inflammatory response (④). Defects in host immune response to or clearing of
microbes may bypass the initial epidermal or sebaceous abnormalities.
Recruitment of more immune cells to the site of disruption and release of pro inflammatory
cytokines and chemokines could further disrupt epidermal differentiation and
barrier function, cause further imbalance of the
skin microbiota, and to allow more yeast metabolites and yeast to penetrate the
epidermal layers, thus trigger sustained inflammation in a vicious circle.
The role of γδ T cells is currently unknown in human SD. Restoration of barrier
function (①), modulating
sebaceous activity (②),
and modulating host immune activity (④) in combination with antifungal treatment (③) may provide more effective
intervention to break the vicious cycle of SD
Environmental factors
SD is
more common and severe in cold and dry climates in winter and improves with sun
exposure.
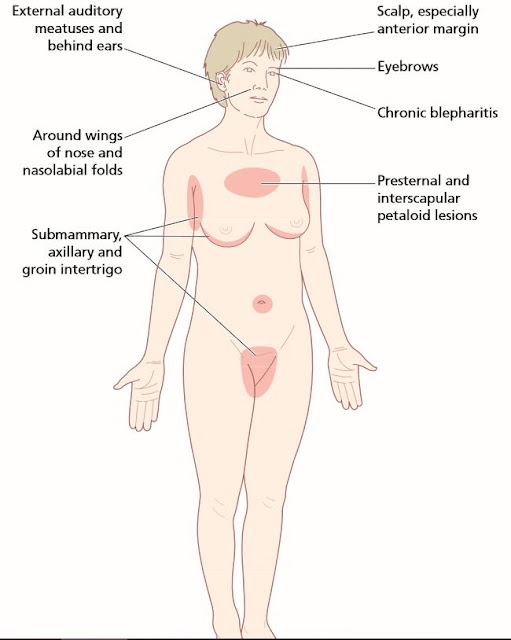
Seborrheic dermatitis: Parts of
the body typically affected
Clinical Features
Seborrheic dermatitis is defined by clinical
parameters, including:
· Red sharply demarcated patches or thin plaques covered with bran-like
flaky greasy adherent scales.
·
A predilection for areas
rich in active sebaceous glands – scalp, facial creases, ears, presternal region and large body folds (inguinal, inframammary, and
axillary). Less commonly involved sites include interscapular, umbilical,
perineum, and the anogenital crease.
·
A mild course with
little or moderate discomfort.
Seborrheic dermatitis is
most often limited in extent, but generalized and even erythrodermic forms can
occur, albeit rarely.
Clinical patterns of
seborrhoeic dermatitis
Adult
Scalp
Dandruff
Inflammatory—may extend onto non-hairy
areas (e.g. post auricular)
Face (may include blepharitis
and conjunctivitis)
Trunk
Petaloid
Pityriasiform
Flexural
Eczematous plaques
Follicular
Generalized (may be erythroderma)
Infantile
Scalp (cradle cap)
Trunk (including flexures
and napkin area)
Adult seborrheic dermatitis
In adults, seborrheic dermatitis
is generally found on the scalp and, usually of milder intensity, on the face;
less often, lesions occur on the central upper chest and the intertriginous
areas. Erythrodermic seborrheic dermatitis has been described as a rarity.
There are several morphological
variants of seborrhoeic dermatitis in the adult form.
Scalp
Dandruff (Pityriasis simplex capillitii) is a common condition and is usually the mildest form and the earliest manifestation of seborrhoeic dermatitis. Most individuals periodically experience a diffuse, slight to moderate, fine dry white scaling of the scalp and terminal hair-bearing areas of the face (beard area), but without significant erythema or irritation. Scales accumulate visibly on dark clothing; this is dandruff. This common condition may be considered the mildest form of seborrheic dermatitis of the scalp. They tend to attribute this condition to a dry scalp and consequently avoid hair washing. Avoidance of washing allows more scales to accumulate and inflammation may occur. As a result yellow bran-like flaky greasy adherent scales may occur on an inflamed base. Patients with minor amounts of dandruff should be encouraged to wash every day or every other day with antidandruff shampoos.
In
seborrheic dermatitis of the scalp, there is inflammation and pruritus in
addition to dandruff. The vertex and parietal regions are predominantly
affected, but in a more diffuse pattern than the discrete plaques of psoriasis.
Towards the forehead, the erythema and scaling are usually sharply demarcated
from uninvolved skin, with the border either at the hairline or slightly
transgressing beyond it
("corona seborrhoica"). Pruritus is usually moderate but may be
intense, particularly in patients with male pattern alopecia; folliculitis,
furuncles, and meibomitis are not uncommon complications, elicited by
scratching and rubbing.
In chronic cases there may be some
degree of hair loss, which is reversible when the inflammation is suppressed.
Behind the ears there may be redness
and greasy scaling, and a crusted fissure often develops in the fold and these
greasy scales and crusts may extend into the adjacent scalp. Both sides of the
pinna, the periauricular region, and the sides of the neck may be involved.
Face
Seborrheic
dermatitis of the facial skin is often strikingly symmetric, affecting the
forehead, medial portions of the eyebrows, the glabella,
eyelashes, upper eyelids, nasolabial folds and lateral aspects of the nose, usually in
association with involvement of the scalp. Lesions
are yellowish-red, with a typical bran-like scale. Hypo pigmentation may be a prominent feature in dark‐skinned
individuals.
Inflammation of the
anterior eyelid margin (anterior blepharitis) may occur in SD and presents as
redness of the lids
margin with flaky debris on the eyelashes,
typically near the base. When this loose debris falls into the eye, it results
in conjunctival irritation and red eye.
Trunk
On the trunk, several forms of seborrhoeic
dermatitis occur. Commonest is the petaloid form (so-called because the lesions
are petal-shaped). This is often seen in men on the front of the chest and in
the interscapular region. The initial lesion is a small, red follicular papule,
covered by a greasy scale. More often, extension and confluence of the
follicular papules gives rise to a figured eruption, consisting of multiple
circinate patches, with a fine branny scaling in their centers, and with
dark-red papules with larger greasy scales at their margins.
A rarer form, involving the trunk and
limbs, is the so-called
pityriasiform type. This is a
generalized erythematosquamous eruption, somewhat similar to, but more
extensive than, pityriasis rosea. In particular it involves the neck up to the
hair margin. It is not particularly pruritic, and it resolves spontaneously,
although somewhat more slowly than does pityriasis rosea. In some patients the
lesions may become psoriasiform.
Flexures
In the flexures, notably in the
axillae, the groins, the anogenital and submammary regions, and the umbilicus,
seborrhoeic dermatitis presents as an intertrigo, with diffuse, sharply
marginated glazed erythema with less scale. Crusted fissures develop in the
folds, and with sweating, secondary infection and inappropriate treatment, a
weeping dermatitis may extend far beyond them.
All show a tendency to chronicity and
recurrence. Occasionally, seborrhoeic dermatitis may become generalized,
resulting in erythroderma.
Adult seborrheic dermatitis has a chronic relapsing course.
Patients feel well and systemic signs are absent. Extensive and severe
seborrheic dermatitis, however, should raise the suspicion of underlying HIV
infection. Among patients with seborrheic dermatitis tested for HIV infection,
2% were found to be positive, frequently in a late stage of their disease. In
patients with Parkinson disease, seborrheic dermatitis is a common finding,
along with seborrhea. Its severity, however, is not correlated with that of the
Parkinson disease. The facial immobility of patients with Parkinson disease
might result in a greater accumulation of sebum on the skin, resulting in a
permissive effect on the growth of Malassezia.
Seborrheic dermatitis may be more common in patients with other causes of
immobility such as cerebrovascular accidents. Rebound flares of seborrheic
dermatitis can follow tapers of systemic corticosteroids.
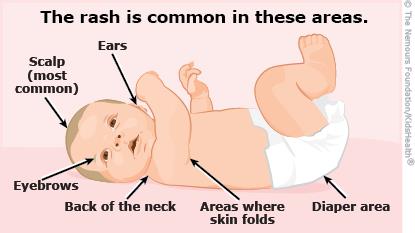
Infantile seborrheic dermatitis
Infantile
SD presents primarily with cradle cap and/or napkin dermatitis. This form usually begins about one week after birth with a
peak incidence at 3 months of age, and may persist for several
months. It corresponds to the time when neonates
produce sebum, which then regresses until puberty. Initially, mild greasy
scales adherent to the vertex and anterior fontanelle regions which may later
extend over the entire scalp. Inflammation with erythema and oozing may finally
result in a coherent scaly and crusty mass covering most of the scalp (“cradle
cap”). Lesions of the axillae, inguinal creases, neck, and retroauricular
folds are often acutely inflamed, oozing, sharply demarcated, and surrounded by
satellite lesions. Superinfection with Candida spp. or
occasionally bacteria (e.g. group A Streptococcus) can
occur. A disseminated eruption of scaly papules with a psoriasiform appearance
(“psoriasiform id reaction”) may develop on the trunk, proximal extremities,
and face in association with exuberant or superinfected seborrheic dermatitis,
especially of the diaper area.
Diagnosis
The diagnosis is usually made on
clinical grounds without the need for diagnostic tests. HIV testing should be
considered in
any patient with severe seborrhoeic dermatitis, particularly in a patient
involved in high-risk activities.
Differential Diagnosis
Infantile seborrheic
dermatitis is distinguished from atopic dermatitis by
its earlier onset, different distribution pattern, and, most importantly, by
the absence of pruritus, irritability and sleeplessness. In contrast to atopic
dermatitis, infants with seborrheic dermatitis generally feed well and are
content.
Irritant
diaper dermatitis is confined to the diaper area and tends to spare the skin
folds.
Candidiasis of
the diaper area can result from colonization with fecal yeast and some infants
have seborrheic dermatitis with a superimposed candidal infection.
Infantile
psoriasis may be difficult to distinguish from psoriasiform seborrheic
dermatitis. Although psoriasiform diaper dermatitis can represent the initial
manifestation of psoriasis, many affected infants do not subsequently develop
psoriasis elsewhere.
When scalp
scaling is present in prepubertal children, the possibility of tinea capitis due to Trichophyton tonsurans should be considered.
Pityriasis
amiantacea is a localized or diffuse inflammatory condition of the scalp
characterized by large plates of thick asbestos-like silvery scales firmly
adherent to both the scalp and hair tufts. This condition can occur at any age,
especially adolescents and young females. Alopecia may result and is generally
non scarring unless secondary scalp infection occurs. Concomitant bacterial
skin infection, mostly Staphylococcus, may result in scarring alopecia,
so early and appropriately treatment is necessary. Young females commonly have concomitant post
auricular scales and fissures.
The most common skin diseases associated with pityriasis amiantacea are
psoriasis (35%), and eczematous conditions like seborrheic dermatitis and
atopic dermatitis (34%). Up to a third of the affected children and adolescents eventually
develop psoriasis.
A number of entities are included in the differential diagnosis
of adult seborrheic dermatitis. Distinction of
seborrheic dermatitis of the scalp from
psoriasis can be difficult. The controversial term sebopsoriasis is
often used in patients when there appears to be an overlap of psoriasis and
seborrheic dermatitis. It tends to localize to the scalp, face, and presternal
chest as seen with seborrheic dermatitis. However, the plaques of
psoriasis tend to be thicker and palpable, brighter pink color with
silvery white scale, more circumscribed and discrete,
less pruritic, and unassociated with seborrhea. In addition, features of
psoriasis may be found elsewhere.
Dry scaling of the scalp, along with dry brittle hair (as opposed
to greasy hair), is a symptom of xerotic skin (e.g. in atopic dermatitis),
frequently mistaken for (and mistreated as) seborrheic dermatitis.
Lichen simplex of the nape of the neck
occurs in females, and can mimic seborrhoeic dermatitis. The thickened plaques
in this condition are, however, intensely irritable.
Seborrheic
dermatitis of the face may closely
resemble both early rosacea and the butterfly lesions of systemic lupus
erythematosus. Lupus erythematosus rarely affects the nasolabial folds and
often has a clearly demonstrable photo distribution. Notably, seborrheic
dermatitis and rosacea frequently coexist.
The differential diagnosis
of seborrheic dermatitis of the trunk includes
pityriasis rosea (but in this latter entity the lesions are ellipsoid in shape,
have collarette-like scaling, and there is no predilection for the central
chest). The
lesions of pityriasiform type of seborrhoeic dermatitis are more widely
distributed, and there is no herald patch.
The brown scaly lesions of pityriasis versicolor
are flatter, more extensive, and less symmetrical than the lesions of petaloid seborrhoeic
dermatitis of the trunk. Microscopy of scrapings quickly establishes the
diagnosis.
In the flexures,
microscopic examination of scrapings from the advancing margin, and examination
under Wood’s light will exclude ringworm infections, candidiasis and
erythrasma.
Clinical
course and prognosis
Generally SD in adults and
adolescence has a chronic and recurrent relapsing course. Consequently the
primary goal of treatment should be control of symptoms like pruritus,
erythema, and scales, rather than cure of the disease. Also patients should be
informed that they need to prepare for a future re-outbreak and avoid
aggravating factors of SD. However, ISD has a benign, self-limited course; ISD spontaneously
disappears by 6-12 months of age. Severe exacerbation with exfoliating
dermatitis may occur, albeit rarely, but its prognosis is usually favorable. ISD
does not progress to adulthood.
Management
Summary of NICE recommendations for the treatment of SD (The
National Institute for Health and Care Excellence)
|
Type of seborrhoeic dermatitis |
First line therapy |
Second line therapy |
Additional therapy |
|
Scalp and beard |
2% ketoconazole shampoo twice a
week for a month, then once or twice a week for symptom control |
Medicated shampoos with zinc
pyrithione, coal tar or salicylic acid |
Topical keratolytic or mineral/olive oil for the removal
of scale and crust Potent topical corticosteroid scalp application for 4
weeks if there is severe scalp itch |
|
Face and body in adults |
Ketoconazole 2% cream o.d./b.d., Use as above for at least
4 weeks, then less frequently |
Mild topical corticosteroids for
1–2 weeks |
Antifungal shampoo, e.g. 2% ketoconazole, as a body wash Hygiene measures for eyelid involvement using cotton buds
moistened with baby shampoo |
|
Severe |
Review diagnosis, consider
specialist referral, HIV testing |
|
|
|
In infants |
Removal of scalp crusts with baby
shampoo and gentle brushing. Overnight soak of petroleum jelly or warmed
vegetable oil if needed. Daily bathing with soap substitute |
Topical imidazole cream:
clotrimazole 1% cream b.d./t.d.s., econazole 1% cream b.d., miconazole 2%
cream b.d. |
Topical corticosteroids not
routinely advised but may be used for certain infants with nappy rash |
Seborrhoeic dermatitis can generally
be suppressed, there is no permanent cure. Long‐term maintenance treatment may be
required but some patients only use treatment intermittently for acute,
symptomatic flares. Topical antifungals are the mainstay of therapy due to
their safety in all ages. Ketoconazole have been the most heavily investigated
topical agent in SD. New formulations may also improve patient choice, such as
2% ketoconazole foam, which was found to be popular and effective as a long‐term treatment of SD for up to 52
weeks. However, some strains of Malassezia globosa and M.
restricta are resistant to azole antifungals and this may be
associated with treatment failure. Ciclopiroxolamine, a broad spectrum antifungal and anti-inflammatory
agent, and a newer azole such as sertaconazole are
also effective topically in treating SD of the scalp as a
shampoo and face as a
cream.
Dandruff is usually treated by the
frequent and regular use of medicated shampoos which act against Malassezia yeasts,
including zinc pyrithione, ketoconazole and various tar shampoos; 1% terbinafine
solution has also been shown to be effective.
For severe dandruff with persistent
scaling or crusting, 5% salicyclic acid ointment may be useful. If secondary bacterial
infection is present or suspected, oral erythromycin or flucloxacillin may be
used.
Acute
forms of seborrhoeic dermatitis on the face, trunk and
ears are treated with topical
corticosteroids in combination with antifungals for their additional anti‐inflammatory effects, with improved
results compared with antifungal monotherapy, which can then be changed to ketoconazole
cream for long-term control. Short courses of low potency topical
glucocorticoids (Class IV or lower) should be used to suppress the initial
inflammation. Hydrocortisone ointment (0.5%) is often effective. Ketoconazole
cream (2%) is possibly a more logical therapy, which has been shown to be
equally effective. Concerns about atrophy limit the
long‐term use of
corticosteroids, especially in delicate sites such as the eyelids. Topical calcineurin
inhibitors are emerging as an effective alternative. Topical calcineurin
inhibitors (pimecrolimus and tacrolimus) have
anti-inflammatory and antifungal (tacrolimus) properties without the long-term
side effects of topical corticosteroid use. They manifest
good effects on SD by blocking calcineurin, thus preventing both inflammatory
cytokines and signaling pathways in T lymphocyte cells. Studies of topical
pimecrolimus and tacrolimus in SD have found that improvement occurred within 2
weeks and that if SD recurred after stopping treatment it was significantly
less severe. Seborrheic dermatitis tends to relapse if a maintenance regimen is
not instituted. As M. furfur has a
slow proliferation rate, an interval of two to several weeks will pass until
relapses appear. The intervals of topical therapy should follow this rhythm. Maintenance treatment with topical calcineurin inhibitors
may be useful in preventing the relapse and twice weekly 0.1% tacrolimus has
been reported to be effective for up to 10 weeks in adult facial SD. Adverse
effects includes mild burning and irritation.
Patients with
seborrheic blepharitis can be treated with warm compresses and washing with
baby shampoo followed by gentle cotton tip debridement of thick scale. Avoid
ocular glucocorticoids. Ophthalmic sodium sulfacetamide ointment can be used
for resistant seborrheic blepharitis.
Other treatments reported to be of benefit in facial SD
include 4% nicotinamide cream and metronidazole 0.75% gel, and these may be
particularly useful in patients with coexistent acne/rosacea.
Frequent washing with soap and water
is helpful, possibly because removal of lipid removes the substrate for the
yeasts.
For unresponsive cases, oral itraconazole
(100 mg daily for up to 21 days) is also effective or itraconazole 200mg for
the first 7 days of the month for several months is a regime used to get
clinical improvement.
Generalized seborrhoeic dermatitis
usually responds to the medications listed above, but in recalcitrant cases
systemic steroids may be required. A 1-week course of prednisolone 0.5 mg/kg body
weight/day usually produces a rapid response, while cautioning the patient of
side effects and informing them of potential rebound flares following
discontinuation of the medication.
Infantile seborrheic dermatitis
(ISD)
The basic
principles of treatment are the same for infants. When ISD involves the diaper
areas, the use of superabsorbent disposable diapers with frequent changes
prevent the aggravation of the symptoms. Soap and alcohol containing compounds
are not recommended in cleaning the diaper lesions.
Infantile
seborrheic dermatitis usually responds satisfactorily to bathing and
application of emollients. Ketoconazole cream (2%) is indicated in more
extensive or persistent cases. Short courses of low-potency topical
corticosteroids may be used initially to suppress inflammation. Mild shampoos
are recommended for the removal of scalp scales and crusts. Avoidance of irritation
(e.g. the use of strong keratolytic shampoos including salicylic acid and
selenium sulfide that are dangerous to neonates because of the possibility of
the percutaneous absorption; and mechanical measures to remove the scales from
the scalp) is important.