Burn
Salient
features
·
Burns
are common in adults and kids; most are small and managed in the outpatient
setting with dressing changes.
·
Serious
burns require inpatient care, ideally in a verified burn center.
·
Large
burns are managed in 4 general phases:
o
Initial
evaluation and resuscitation.
o
Wound
debridement and biologic closure.
o
Rehabilitation
and reconstruction.
o
Long-term
outcome quality tends to be very good in patients surviving large burns.
|
CLINICAL AND PATHOLOGIC FEATURES OF THERMAL BURNS |
|||
|
Type |
Depth |
Clinical features |
Pathology |
|
First
degree |
Epidermis
only |
Pain,
tenderness, erythema |
Upper
epidermal necrosis |
|
Second
degree – superficial |
Epidermis
and superficial dermis |
Severe
pain, tenderness, serous or hemorrhagic bullae, deep rubor, erosion, and
exudation |
More
extensive epidermal necrosis with vertical elongation of keratinocytes |
|
Second
degree – deep |
Epidermis
and most of dermis destroyed, including deep follicular structures |
Intense
pain but reduced sensation, deep red to pale and speckled in color |
Destruction
of entire epidermis, dermal collagen, and most of adnexal structures |
|
Third
degree |
Full-thickness
epidermal and dermal destruction |
Dry,
hard, charred, non-blanching, insensitive areas of coagulation necrosis |
Necrosis
of entire epidermis and dermis, with extension into subcutis |
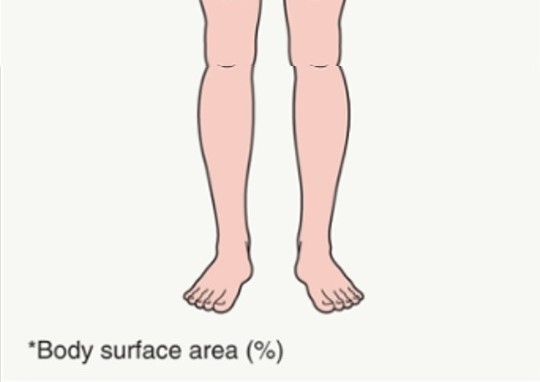
In adults, an estimate of burn extent is often
based upon this surface area distribution chart. Infants and children have a
relatively increased head: trunk surface area ratio. These estimates are also
used for primary cutaneous disorders.
Management
Initial
management of burn victims includes assessment of cardiopulmonary status as
well as the extent and depth of the burn.
For first- and second-degree burns, the burn wound itself should
initially be rinsed with cold running water for 20 minutes in order to ease
pain, reduce heat, and reduce burn depth. Then the wound should be gently
cleansed to remove any foreign material. The next step is prevention of
infection, followed by creation of a proper healing environment. Topical antimicrobial
agents shown to be effective in burn wound care include silver sulfadiazine,
mafenide acetate, and silver nitrate. Silver sulfadiazine has gained wide
acceptance for both pediatric and adult burn treatment, but it is known to be
cytotoxic and percutaneous absorption can lead to leukopenia. Silver
sulfadiazine also produces a pseudoeschar that may interfere with burn depth
assessment and prolonged application may lead to localized argyria (skin turns
blue or blue-grey). Some experts therefore prefer
mafenide acetate.
While
superficial wounds may require minimal additional therapy, deeper burn wounds
need more aggressive therapy, with the standard approach being serial excision
and autografting (if there are sufficient donor sites). Third-degree burns are
excised early, with indeterminate and deep second-degree wounds delayed until
maximum depth and extent are known. Biologic dressings (e.g. pig skin, human
allograft) were popular for several years, but have been largely displaced due
to higher infection risk and poorer healing. Skin substitutes such as acellular
human dermal matrix (Alloderm®), bilaminar
bovine collagen–shark chondroitin sulfate (Integra®),
and cultured epithelial autografts are increasingly being utilized.
1st0
burn: with intact epidermis require a bland
ointment.
Topical corticosteroids used to relief inflammation.
Neither topical nor systemic antibiotics are
required for 1st0 burn.
2nd0
burn: clean and dress.
Aspiration or drainage of fluid, intact blisters
left for a day or two as a natural wound dressing. Broken blisters or other
dead tissues should be removed. Dressing should consist of Vaseline gauze
placed on the affected skin, followed by gauze pads and easily stretched
dressing. Topical antibiotic such as silver sulfadiazine cream is often used.
3rd0
burn: beyond the scope of dermatologist.
Broad spectrum prophylactic antibiotics are
given and then adjusted according to C/s reports.
Pain therapy.
High calories diets and give trace elements
such as Zinc and Vit C, both of which can be quickly lost.
2nd0 burn and deeper: scars with
contractures are major problem, especially in younger patients.
Scars can be minimized with early physical
therapy.
Keloids can be inhibited by the early use of
pressure garments or dressings for 6 months or even more in children.
Good skin care with non sensitizing ointments
to avoid dryness and fragility. Scars and contractures corrections are best
left in the hands of plastic surgeons.