Melasma
Salient features
· At least 90% of
patients are women
· Increased prevalence
in individuals who are Hispanic, or of Asian or African descent
· Most common location
is the face, followed by the forearms
· Symmetric patches of
hyper pigmentation with irregular borders due to increased melanin within the
epidermis and/or dermis
Introduction and epidemiology
Melasma is a common acquired disorder characterized
by hyper pigmented macules and patches occurring most commonly on sun exposed
area of the face in genetically predisposed women and men. It is most prevalent among women,
especially those of reproductive age.10% of patients are men. Mostly starts between the ages of 20 and 40 years. The prevalence of melasma increases with age in both men and women. Exacerbating
factors include sun exposure, pregnancy, and use of oral contraceptives.
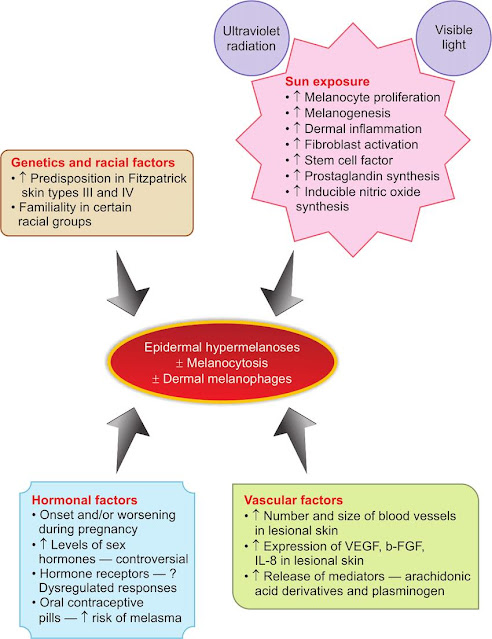
Etiopathogenesis
Major
etiological factors of melasma with mechanisms associated with them
Although
the exact pathogenesis of melasma is unknown, but genetic and hormonal
influences in combination with UV radiation are important. Sun exposure is the primary trigger. Melasma patients pigment more easily with UV exposure.
It is hypothesized that following
exposure to UV irradiation (or another inducer), hyper functional melanocytes
within involved skin produce increased amounts of melanin. The key role of UV
irradiation is supported by fading of lesions during winter months and a
distribution pattern demonstrating involvement of sun-exposed regions and
sparing of relatively sun-protected sites such as the philtrum. People with
darker skin types are more frequently affected. Pregnancy and oral
contraceptives have been linked to increased skin pigmentation. It has been
speculated that this is due to increased levels of estrogen and progesterone
stimulating the activity of melanocytes. Melasma is common in the third
trimester of pregnancy when levels of estrogen, progesterone and MSH are
elevated. Melasma is more common and severe in women than men.
Melasma may be seen in other endocrinologic disorders, such as mild ovarian dysfunction,
ovarian tumors and autoimmune thyroid disease. Medications like (e.g.
phenytoin, hydantoins,
phototoxic
drugs and oral finasteride) and some cosmetics also have the potential to
aggravate melasma. The number of
melanocytes is not increased but they become enlarged and more dendritic,
suggesting a hypermetabolic state. This is reflected by increased melanin
deposition in the epidermis and dermis. Increased
expression of KIT and stem cell factor within the lesional epidermis and
dermis, respectively, may play a role in the hyper pigmentation of melasma.
Genetics
No
specific genes have as yet been identified but a family history is common
(around 30%).
Clinical features
( (a ) Centro facial
(b) Malar
(c) Mandibular
The lesions are sharply defined
brown color macules and patches with irregular borders, photo distribution
usually on the face, often coalescing in a reticular pattern. The pigmentation
is usually
uniform but also blotchy. The areas of hyper melanosis are usually bilateral and are frequently symmetrical in three classic patterns: (1) centrofacial
(most common), involving the forehead, cheeks, nose, upper lip (sparing the
philtrum and nasolabial folds) and chin; (2) malar, affecting the cheeks
and nose; and (3) mandibular, along the jawline, patients are often
postmenopausal. The centrofacial and malar patterns comprise the
majority of patients. Lesions
often first appear or are accentuated following exposure to UV irradiation or
during pregnancy. In lightly pigmented individuals, this “mask of pregnancy”
frequently diminishes or disappears after parturition, but it tends to persist
in women with more darkly pigmented skin.
Less common sites include the
extensor aspect of the forearms (d) and mid upper chest (e).
Localization of pigmentation (wood’s
light)
Three
histologic patterns of pigmentation have been described: epidermal, dermal, and
mixed. Perform a Wood’s lamp examination to identify the depth of the melanin
pigmentation. There are three types based on Wood’s light examination: (1) The
epidermal type has increased levels of melanin in the basal, suprabasal, and
stratum corneum layers; the pigmentation is intensified by Wood’s light
examination. (2) The dermal type does not show enhancement with the Wood’s
light; melanophages are found in the superficial and mid dermis. (3) A
mixed-type epidermal and dermal pigment type shows no or slight enhancement
with the Wood’s light. The epidermal type responds to depigmenting agents; the
dermal pigmentation resists the action of bleaching agents.
Melasma—Clinical Types and Patterns
|
Type |
Clinical |
Wood’s
light examination |
Histology |
|
Epidermal |
Light brown
in color, Well
defined border, Responds
well to treatment |
Enhancement
of pigmentation |
Melanin
increase in basal, suprabasal, and stratum corneum layers |
|
Dermal |
Ashen or
bluish gray in coor, Ill-defined
border, Responds
poorly to treatment |
No
enhancement of pigmentation |
Melanin-laden
macrophages in a perivascular location found in superficial and mid-dermis |
|
Mixed |
Dark brown
in color, Most
common type, Partial
improvement with treatment |
Enhancement
of pigmentation in some places |
Melanin
deposition found in epidermis and dermis |
Treatment
Treatment
of melasma can be difficult due to the refractory and recurrent nature of the
condition. Diligent sun protection and patient motivation are necessary for
any melasma treatment regimen to be successful. For epidermal melasma, 2 months
of therapy are typically required to initiate lightening and 6 months of
treatment are often needed to achieve satisfactory results. Treatments
include hypo pigmenting agents, chemical peels, and lasers.
Hypo pigmenting Agents
|
Class |
Treatment |
Mechanism of action |
|
Phenolic hypo pigmenting agent |
Hydroquinone |
Inhibits tyrosinase, leading to decreased
conversion of dopa to melanin |
|
Nonphenolic hypo pigmenting agent |
Glycolic acid (alpha-hydroxyacid) |
Thins stratum corneum, disperses melanin in
basal layer of epidermis, enhances epidermolysis, increases collagen
synthesis in dermis |
|
Nonphenolic hypo pigmenting agent |
Kojic acid (produced by fungus Aspergillus
oryzae) |
Inhibitor of tyrosinase |
|
Nonphenolic hypo pigmenting agent |
Azelaic acid (saturated dicarboxylic acid) |
Reversible inhibitor of tyrosinase;
inhibits mitochondrial respiration |
|
Nonphenolic hypo pigmenting agent |
Tretinoin (retinoid) |
Enhances keratinocyte proliferation and
increases epidermal cell turnover |
|
Chemical peel |
Glycolic acid peel |
Thins stratum corneum, disperses melanin in
basal layer of epidermis, enhances epidermolysis, increases collagen
synthesis in dermis |
|
Laser |
Pulsed CO2 laser with Q-switch
alexandrite laser |
Pulsed CO2 laser; resurfacing of
epidermis Q-switch alexandrite laser; photo thermolysis of melanosomes |
|
Light |
Intense pulsed light |
High-intensity pulses of broad-band light
that are different from narrow-band light of lasers; causes thermal damage;
does not damage surface |
Managing Melasma
|
Primary agent |
Alternative agents |
|
|
First-line |
Triple combination products containing
hydroquinone, a retinoid, and a fluorinated steroid (Tri-Luma) once daily, or |
Azelaic acid |
|
Adjunctive treatment |
Ascorbic acid |
Kojic acid |
|
Second-line |
Glycolic acid peels every 4-6 week starting
at 30% and increasing in concentration as tolerated |
|
|
Third-line |
Fractional laser therapy |
Intense pulsed light |
First-line
therapy is fixed triple combinations (e.g., Tri-Luma cream [fluocinolone acetonide
0.01%, hydroquinone 4%, tretinoin 0.05%]). Patients who do not tolerate triple
combination therapy are treated with single agents (4% hydroquinone or azelaic
acid) or combinations of these agents. Lasers and intense pulsed light may be helpful
in patients who fail topical creams, but can also result in further unwanted
hyper pigmentation. Sometimes, melisma slowly disappears, after discontinuation
of hormonal stimulus and/or careful sun avoidance.
Sun
protection
UV radiation
has a significant effect on the pathogenesis of melasma. Sun exposure must be
minimized. Sunscreens that block both UVA and UVB light should be used.
Titanium dioxide– and zinc oxide–containing sunscreens reflect UVA and UVB. Broad-spectrum
sun protection enhances the efficacy of hydroquinone. A broad-spectrum UVA- and
UVB-protective sunscreen with an SPF of at least 30 along with a physical
block, such as titanium dioxide or zinc oxide, should be used.
Camouflage
makeup
Camouflage
makeup is an important component in the treatment of melasma. Dermablend,
Covermark, and Cover FX come in a range of shades and offer heavy coverage to
help even out skin tone.
Hypo pigmenting
agents
Hydroquinone
is the most effective topically applied bleaching agent. This agent is available in 2% concentrations
without prescription and by prescription in 3% and 4% concentrations. The
medication should be applied twice daily—in the morning and before bedtime. The
mechanisms of action of hydroquinone include: (1) competing with tyrosine as a
substrate for tyrosinase, the initial enzyme in the melanin biosynthetic
pathway that converts tyrosine to dopaquinone; and (2) selective damage to
melanosomes and melanocytes. Side effects include irritant and allergic contact
dermatitis, post inflammatory hyper pigmentation, and exogenous ochronosis. The
latter side effect is uncommon and is usually caused by prolonged use of
hydroquinone at a concentration >2%. As it is an irritant and a sensitizer,
skin should be tested for sensitivity before use by applying a small amount to
the cheek or arm once each day for 2 days (open patch testing). The development
of erythema or vesiculation indicates an allergic reaction and precludes
further use. These preparations must be used for months and in many cases
result in gradual depigmentation. Skin must be protected with broad-spectrum
sunscreens both during and after treatment.
Combination
products (most effective treatment)
Tri-Luma
cream is a combination product containing 4.0% hydroquinone, 0.05% tretinoin,
and 0.01% fluocinolone acetonide. It is more effective than any of the single
agent treatments. The recommended course of therapy is daily for 8 weeks.
Significant results have been seen after the first 4 weeks of treatment. After
8 weeks of treatment, 13% to 38% of the patients achieved clearing of melasma.
The cream is safe in the treatment of moderate to severe melasma for up to 24
weeks when used intermittently. Treatment may be repeated. Tretinoin enhances
the epidermal penetration of hydroquinone and prevents the oxidation of
hydroquinone. The topical steroid reduces irritation from the other two
ingredients and inhibits melanin synthesis.
Azelaic
acid
Azelaic acid
is used to treat acne and melasma. It has selective effects on hyperactive and
abnormal melanocytes. It is reported to be as effective as 4% hydroquinone.
Azelaic acid with tretinoin causes more skin lightening after 3 months than
azelaic acid alone. Azelaic acid is applied twice daily for several (up to 8)
months; lightening starts after 1 to 2 months. Both 20% azelaic acid and 4%
hydroquinone are equally effective. There is initial and transitory irritation
but the medication is well tolerated and safe for use during pregnancy.
Kojic
acid
Kojic acid
(KA) is an antibiotic produced by many species of Aspergillus and Penicillium
that inhibits tyrosinase. KA is used in 1% to 4% preparations, twice daily for
2 months; higher concentrations do not improve its depigmenting activity.
Contact allergy is reported. Kojic
acid in combination with hydroquinone gives better result.
Ascorbic
acid
Ascorbic
acid (vitamin C) containing creams cause skin lighting with less irritation
than hydroquinone. It may be a useful adjunctive treatment in patients who
cannot tolerate the irritation of hydroquinone.
Chemical
peels
Superficial,
medium, and deep chemical peels are used to treat melasma in lighter-complexion
people. Trichloroacetic acid and glycolic acid have been used; they are
somewhat effective. Darker- complexion individuals are poor candidates for
chemical peels because post inflammatory hyper pigmentation frequently occurs.
Lasers
Fractional
resurfacing creates microzones of thermal damage. It does not cause full-thickness
epidermal wounds. The laser is approved by the FDA for the treatment of
melasma.
Intense
pulsed light (IPL)
IPL
treatment produces modest improvement. Epidermal melasma responds. Individuals
with deep pigmented lesions (including mixed melasma) show fair or poor
clearance
|
TREATMENT
OPTIONS FOR MELASMA |
|
Recommendations
for all patients |
|
Avoidance of sun exposure and tanning beds Daily use of broad-spectrum sunscreen (ideally SPF
≥30 with physical blocker such as zinc oxide or titanium dioxide) Sun-protective hats and clothing Camouflage makeup ·
Change
oral contraceptive to an alternative low‐oestrogen preparation, or change
to a different form of contraception ·
Avoidance
of scented cosmetic products and phototoxic drugs |
|
Active
treatment*,** |
|
1. First-line topical
therapies Triple combination of HQ + retinoid + corticosteroid§ at bedtime 4% HQ daily, typically at bedtime Azelaic acid (15–20%) 2. Adjunctive topical
therapies L-ascorbic acid (10–15%) Kojic acid (1–4%) 3. Second-line
therapies Glycolic (start at 30% and increase as tolerated) or
salicylic acid peels (20–30%) every 4–6 weeks 4. Third-line therapies¶ Fractional laser Intense pulsed light (IPL) |
|
Long-term
maintenance |
|
Continue daily sunscreen and sun-protective measures
(see above) Topical retinoid Topical α-hydroxy acid (e.g. glycolic acid
cream) Other topicals, e.g. L-ascorbic acid (10–15%), azelaic acid (15–20%), or kojic acid (1–4%) |
* Results
from topical treatments may take up to 6 months to appreciate; depending on the
patient, HQ or a combination HQ + retinoid + corticosteroid are typically used
daily for 2–4 months and then decreased in frequency to 1–2 times per week;
prolonged daily use can result in side effects such as perioral dermatitis and
atrophy (corticosteroid) or exogenous ochronosis
** While
topical HQ can cause allergic contact dermatitis, all topical agents may lead
to irritant contact dermatitis, which can worsen the dyspigmentation; if this
is a concern, can test on a small, non-facial site prior to widespread facial
application.
§ Typically
a class 5–7 topical corticosteroid is used
¶ Potential
risk of post-procedural dyspigmentation; a small test site should be performed
prior to widespread facial laser or light therapy.