Erythema multiforme
Salient features
|
|
|
|
|
|
|
|
|
Introduction
Erythema
multiforme (EM) is an acute, self-limited, usually mild, and often relapsing
mucocutaneous syndrome
resulting from cell‐mediated hypersensitivity reaction most commonly to
infection, less
commonly to drugs, characterized by the abrupt onset
of symmetric fixed red papules, some of which evolve into typical and/or
occasionally “atypical” papular target lesion. Most cases are
related to infections (herpes simplex virus [HSV] (facial or genital) and Mycoplasma
pneumoniae). Medications are not a common cause, in
contrast to the spectrum of drug-induced epidermal necrolysis. Two forms of EM are recognized
– EM minor and EM major. Both are characterized by the same type of elementary
lesions (targets), but are distinguished by the presence or absence of mucosal
involvement and systemic symptoms.
Erythema Multiforme
Subtypes
|
·
Erythema multiforme minor: EMm C/F:
typical targets, acral skin and lip involvement, no mucosal erosions. Associated
etiology: HSV, other infections ·
Erythema multiforme major: EMM C/F:
typical targets, acral skin involvement, mucosal erosions of at least two
mucosal sites Associated
etiology: HSV, other infections ·
Atypical EMM C/F:
giant targets, central distribution, prominent mucosal erosions. Associated
etiology: mycoplasma pneumonia, HSV ·
Mucosal EMM C/F: no
skin involvement, prominent mucosal erosions. Associated
etiology: mycoplasma pneumonia. ·
Continuous or persistent EM C/F:
typical targets, acral skin involvement, few mucosal erosions, overlapping
recurrences Associated etiology: HSV,
idiopathic |
Epidemiology
Age of Onset
50% is under 20 years.
Sex
More frequent in males than in females.
Etiology
The etiology of EM is
unclear in most patients, but appears to be an immunological hypersensitivity
reaction with the appearance of cytotoxic effector cells (CD8+ T lymphocytes)
in the epithelium, inducing apoptosis of scattered keratinocytes and leading to
satellite cell necrosis.
Predisposing factors
There may be a genetic
predisposition, with associations of recurrent EM with HLA‐B15 (B62), HLA‐B35,
HLA‐A33, HLA‐DR53
and HLA‐DQB1*0301. HLA‐DQ3
has been proven to be especially related to recurrent EM and may be a helpful
marker for distinguishing this herpes‐associated EM from other
diseases with EM‐like lesions. Patients with extensive mucosal
involvement may have the rare HLA allele DQB1*0402.
Triggering factors
In
up to half of cases, there is no known provoking factor. The most common
association is with a preceding herpes simplex infection (facial or genital) or
with a Mycoplasma infection, especially when conjuctival and
corneal involvement occurs; other viral or bacterial infections and vaccination
have also been incriminated
The
reaction is triggered by the following:
- Infective agents, particularly HSV (herpes‐associated EM), which is implicated in 70% of recurrent EM. Bacteria (Mycoplasma pneumoniae, and many others), other viruses, fungi or parasites are less commonly implicated.
- Drugs such as sulphonamides (e.g. co‐trimoxazole), cephalosporins, aminopenicillins, quinolones, barbiturates, oxicam non‐steroidal anti‐inflammatory drugs, anticonvulsants, protease inhibitors, allopurinol and many others may trigger severe EM or toxic epidermal necrolysis in particular.
- Food additives or chemicals such as benzoates, nitrobenzene, perfumes, terpenes.
- Immune conditions such as bacilli Calmette–Guérin (BCG) or hepatitis B immunization, sarcoidosis, GVHD, inflammatory bowel disease, polyarteritis nodosa or systemic lupus erythematosus (SLE).
- Idiopathic probably also due to undetected herpes simplex or Mycoplasma.
Pathophysiology
The pathophysiology of erythema
multiforme (EM) is still not completely understood, but it is probably
immunologically mediated and appears to involve a hypersensitivity reaction
that can be triggered by a variety of stimuli, particularly viral, bacterial,
or chemical products.
Cell-mediated immunity
appears to be responsible for the destruction of epithelial cells. Early in the
disease process, the epidermis becomes infiltrated with CD8 T lymphocytes and
macrophages, whereas the dermis displays a slight influx of CD4 lymphocytes.
These immunologically active cells are not present in sufficient numbers to be
directly responsible for epithelial cell death. Instead, they release
diffusible cytokines, which mediate the inflammatory reaction and resultant
apoptosis of epithelial cells. In some patients, circulating T cells
transiently demonstrate (for < 30 d) a T-helper cell type 1 (TH1) cytokine
response (interferon [IFN] gamma, tumor necrosis factor [TNF] alpha,
interleukin [IL] 2). Results of immunohistochemical analysis have also shown
lesion blister fluid to contain TNF, an important proinflammatory cytokine.
In
the majority of children and adults with EM, the disease is precipitated by HSV
types 1 and 2. Preceding herpes labialis is noted in ~50% of patients with EM.
Herpes labialis may precede the onset of the cutaneous lesions, occur
simultaneously, or be evident after the target lesions of EM have appeared.
Most commonly, herpes labialis precedes target lesions of EM by 3–14 days. It
is presumed that most cases in children and young adults are due to HSV type 1,
but documented cases of HSV type 2 in adolescents and young adults have been
reported.
Not
only are HSV-encoded proteins found within affected epidermis, but HSV DNA can
be detected within the early red papules or the outer zone of target lesions in
80% of individuals with EM. The presence of fragments of HSV DNA (most often
comprised of sequences that encode its DNA polymerase) within the cutaneous
lesions, as well as the expression of virally encoded antigens on
keratinocytes, may be interpreted as evidence for replicating HSV within
affected skin sites. However, replication must be at a low level, because
usually HSV cannot be cultured from EM lesions.
The
inflammation within cutaneous lesions is believed to be a part of an
HSV-specific host response. Individuals with HSV-associated EM have normal
immunity to HSV, but may have difficulty clearing the virus from infected
cells; within sites of cutaneous lesions, HSV DNA may persist for 3 months
after a lesion has healed. Development of cutaneous lesions is initiated by the
expression of HSV DNA sequences within the skin, followed by the recruitment of
virus-specific T helper type 1 (Th1) cells that produce interferon-γ in response to viral antigens within the skin.
An “autoimmune” response is then thought to result from the recruitment of T
cells that respond to autoantigens released by lysed/apoptotic viral
antigen-containing cells. More recently it was shown that the HSV DNA fragments
are transported (by peripheral blood CD34+ Langerhans
cell precursors) to the sites where EM skin lesions will develop prior to each
eruption.
While
HSV is the predominant cause of EM, there are other associated infectious
agents. In particular, a severe acro-mucosal presentation with mucositis,
conjunctivitis, and targetoid or bullous skin eruptions can be seen in patients
with M. pneumoniae infections,
primarily community-acquired pneumonia. This variant occurs most commonly in young
boys and adolescents. M. pneumoniae has
been cultured from the bullae in patients with EM-like skin reactions,
suggesting an etiologic role.
Clinical features
Clinical criteria allow the distinction of
both forms of EM from SJS/TEN in the vast majority of patients. These clinical
criteria are as follows: (1) the type of elementary skin lesion; (2) the
distribution of skin lesions (topography); (3) the presence or absence of overt
mucosal lesions; and (4) the presence or absence of systemic symptoms.
|
COMPARISON OF ERYTHEMA MULTIFORME (EM) MINOR, EM MAJOR AND
STEVENS–JOHNSON SYNDROME (SJS) |
||||||||||||||||||||||||||||||
|
|
Type of skin lesions |
Distribution |
Mucosal involvement |
Systemic symptoms |
Progression to TEN |
Precipitating factors |
||||||||||||||||||||||||
|
EM minor |
|
|
Absent or mild |
Absent |
No |
|
||||||||||||||||||||||||
|
EM major |
|
|
Severe |
Present |
No |
|
||||||||||||||||||||||||
|
SJS |
|
|
Severe |
Present |
Possible |
|
||||||||||||||||||||||||
Elementary skin lesion
The
characteristic elementary skin lesion of EM is the typical target lesion.
The latter measures <3 cm in diameter, has a regular round, circle shape papule
or plaque and a well-defined border, and it consists of at least three distinct
concentric zones: (1) a central area of dusky erythema or purpura; that has
evidence of damage to the epidermis (2) a middle paler zone of edema; and (3) an
outer ring of erythematous halo. The central area may be bullous. Over time,
the lesion may resemble a “bull’s eye”.
While
early target lesions often have a central dusky zone and a red outer zone
(“iris” lesion), they can evolve to three zones of color change. The
individual lesions begin as sharply marginated, erythematous macules, which
become raised, edematous papules over 24–48 h. The lesions may reach several centimeters
in diameter. Typically, a ring of erythema forms around the periphery, and
centrally the lesions become flatter, purpuric, and dusky, they can evolve to classic
“target” lesion with three zones of color change. Each concentric ring within
the target lesion most likely represents one of a sequence of events of the
same ongoing pathologic process. This may explain why
some patients have only a limited number of fully developed, typical targets
amidst a number of target lesions that are not yet typical or fully evolved,
while in others all the lesions are at the same stage of development, thus
creating a monomorphic clinical appearance. Given the possibility that only a
few typical target lesions may be present, a complete skin examination is
essential.
In
EM, elevated atypical papular target lesions can either accompany
typical target lesions or constitute the primary cutaneous lesion. Raised
atypical target lesions are ill-defined, round, palpable lesions with only two
zones including a central raised edematous area with an erythematous border. They
must be distinguished from the flat (macular) atypical targets that are seen in
SJS or TEN, but not EM. The latter are defined as round lesions, but with only
two zones and/or a poorly defined border, as well as being non-palpable (with
the exception of a potential central vesicle or bulla).
Distribution of skin lesions (topography)
Although
there is considerable variation from individual to individual, numerous lesions
are usually present. In general, lesions of EM develop preferentially on the extremities
and the face; target lesions favor the upper extremities, as does the entire eruption of EM. Typical
targets are best observed on the palms and soles. Lesions often first appear
acrally and then spread centripetally in a symmetric distribution, with
initial involvement most frequently on the dorsal hands.
The dorsal feet,
extensor aspect of the forearms, elbows, knees, palms and soles typically
become involved, less commonly the face.
In about 10% of cases, more widespread lesions occur on the trunk. Often
the hands are selectively involved. Thus, the typical distribution is acral. In
addition, lesions tend to be grouped, especially on the elbows or knees
The
Koebner phenomenon may be observed, with target lesions appearing within areas of
cutaneous injury such as scratches or within areas of sunburn. The injury must precede the onset of the EM eruption
because the Koebner phenomenon does not occur once the EM lesions have
appeared. Although patients occasionally report burning and itching, the eruption
is usually asymptomatic.
Predilection sites and distribution of EM
Mucous Membrane Lesions
Most patients with EM
(70%), of either minor or major forms, have oral lesions. The oral mucosa may
be involved alone or in association with skin lesions. EM minor affects one
mucosa and EM major affects two or more mucous membranes.
Predilection sites for mucosal
lesions are the lips, on both cutaneous and mucosal sides, non attached
gingivae, and the ventral side of the tongue. The hard palate is usually
spared, as are the attached gingivae. On the cutaneous part of the lips,
identifiable target lesions may be discernible. On the mucosa proper, lesions begin as erythematous areas that blister
and break down to irregular extensive painful erosions with extensive
surrounding erythema. The labial mucosa is often involved, and a serosanguinous
exudate leads to crusting of the swollen lips. The process may rarely extend to
the throat, larynx, and even the trachea and bronchi.
Eye
involvement begins with pain and bilateral conjunctivitis in which vesicles and
erosions can occur. In children, ocular lesions appear to be more frequent and
more severe in M. pneumoniae- associated cases.
Mucosal erosions plus
typical or atypical raised targets and epidermal detachment involving less than
10% of the body surface and usually located on the extremities and/or the face
characterize herpes simplex‐induced EM major.
Mucosal erosions plus
widespread distribution of flat atypical targets or purpuric macules and
epithelial detachment involving less than 10% of body surface on the trunk,
face and extremities are characteristic of drug‐induced
Stevens–Johnson syndrome.
Systemic
symptoms
Systemic
symptoms are almost always present in EM major and absent or limited in EM
minor. In EM major, the systemic symptoms that usually precede and accompany
the skin lesions are fever and asthenia of varying
degrees. Arthralgias with joint swelling have occasionally been
described, as has pulmonary involvement resembling atypical pneumonia. Whether
the latter is a pulmonary manifestation of EM versus one of the associated
infections such as M. pneumoniae is unclear. Renal, hepatic and hematologic abnormalities
in the context of EM major are rare.
Clinical types
Mild
Forms (EM Minor)
This accounts for
approximately 80% of cases. Mucous membranes are usually spared or minimally
affected, and often limited to the lip. Vesicles may be present but no bullae or systemic symptoms.
Eruption usually confined to extremities and face. Typical EM minor is
usually associated with a preceding orolabial HSV infection. HAEM lesions
appear 1–3 weeks (average 10 days) after the herpes outbreak. The majority of
idiopathic cases of EM minor are associated with recurrent HSV infections, and
patients may be successfully treated with suppressive antiviral regimens.
Localized vesiculobullous form
This form is
intermediate in severity. The skin lesions present as erythematous macules or
plaques, often with a central bulla and multiple concentric
vesicular rings
(herpes iris of Bateman). Mucous membranes are quite often involved. In this
type, the skin lesions tend to occur in the classic acral distribution, but may
be few in number. This pattern may be
more frequent in Mycoplasma pneumoniae-related cases of atypical EMM.
Severe Forms (EM Major)
This is a severe illness
associated with more extensive target lesions and mucous membrane involvement.
The onset is usually sudden, although there may be a prodromal systemic illness
of 1–13 days before the eruption appears.
It occurs in all ages, is centered on the extremities and face,
but more often than EM minor may include truncal lesions; severe, extensive,
tendency to become confluent and bullous, positive Nikolsky sign in
erythematous lesions. It typically shows a cockade-like erythema on the
extensor surface of the extremities as well as trunk involving less than 10% of
the body surface area. Mucous
membrane disease is prominent and often involves not only the oral mucosa and
lips, but the genitalia and ocular mucosa as well. EM major is associated with Mycoplasma infections, although minority
may result from herpes simplex and reaction to drugs.
Fuchs syndrome is a clinical
variant of EMM, with exclusive involvement of conjunctivae and oral mucosa
Generalized EMM with
cockade-like erythema
Fuchs syndrome: Extensive erosions of the
conjunctiva and the oral mucosa without involvement of other skin
Rowell syndrome
This syndrome comprises lupus erythematosus associated with EM‐like skin lesions, and immunological findings
of speckled antinuclear antibodies, anti‐La or anti‐Ro
antibodies, and a positive test for rheumatoid factor
Natural
history
In
EM, a history of an abrupt onset of skin lesions is obtained, with almost all
of the lesions appearing within 24 hours and full development by 72 hours and the
individual lesions remain fixed at the same site for 7 days or longer. Often there are a limited number
of lesions, but up to hundreds may form. In most cases, EM affects well under 10% of the
body surface area.
For
most individuals with EM, the episode lasts 2 weeks and heals without sequelae;
one possible rare exception is ocular sequelae in the setting of EM major,
which may occur if adequate eye care is not promptly instituted. Occasionally,
post-inflammatory hyper- or hypopigmentation is seen. Patients with EM usually
have an uncomplicated clinical course, although recurrences, in the case of
HSV-associated EM, are quite common. Most individuals with recurrent
HSV-associated EM have one or two episodes a year, an exception being those
receiving immunosuppressive drugs such as oral corticosteroids which may be
associated with more frequent and longer episodes of EM. These individuals may
have five or six episodes per year or even almost continuous disease in which
one attack has not completely resolved before another occurs. The incidence of
secondary bacterial infections also increases in the setting of prolonged
corticosteroid use.
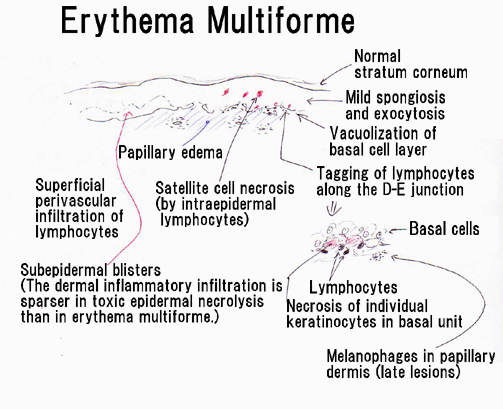
Pathology
EM
is a clinicopathologic, not a purely histologic, diagnosis. Histologic findings
are characteristic, but not specific, and are most useful for excluding
entities in the differential diagnosis such as lupus erythematosus (LE) and
vasculitis.
In EM, the keratinocyte is the target of the inflammatory insult, with
apoptosis of individual keratinocytes being the earliest pathologic finding. Early lesions of EM exhibit
lymphocyte accumulation at the dermal–epidermal interface, with exocytosis into
the epidermis, lymphocytes attached to scattered necrotic keratinocytes
(satellite cell necrosis), spongiosis, vacuolar degeneration of the basal cell
layer, and focal junctional and subepidermal cleft formation. The papillary
dermis may be edematous and a dense perivascular infiltrate
of lymphocytes is also present, which is more abundant in older lesions. The
vessels are ectatic with swollen endothelial cells; there may be extravasated
erythrocytes and eosinophils. Immunofluorescence findings are negative or nonspecific.
In advanced lesions subepidermal blister formation may occur, but necrosis
rarely involves the entire epidermis. In late lesions, melanophages may be
prominent.
Specific
HSV antigens have been detected within lesional keratinocytes by immunofluorescence,
and HSV genomic DNA has been detected by PCR amplification of skin biopsy
specimens.
Compared
to SJS, the dermal inflammation component is more prominent in EM and the
epidermal “necrolysis” component is more discrete. Large areas of full-thickness
epidermal necrosis are not seen in EM.
|
DIFFERENCES
BETWEEN URTICARIA AND ERYTHEMA MULTIFORME |
|
|
Urticaria |
Erythema
multiforme |
|
Central
zone is normal skin |
Central
zone is damaged skin (dusky, bullous or crusted) |
|
Lesions
are transient, lasting less than 24 hours |
Lesions
“fixed” for at least 7 days |
|
New
lesions appear daily |
All
lesions appear within first 72 hours |
|
Associated
with swelling of face, hands or feet (angioedema) |
No edema |
DIAGNOSIS
The target-like lesion and the symmetry are quite typical.
Treatment
Treatment of
EM is determined by its cause and extent. Therapeutic
options include topical and systemic treatment of the acute eruption as well as
prophylactic treatment of recurrent disease. EM minor is
generally related to HSV, and prevention of herpetic outbreaks is central to
control of the subsequent episodes of EM. A sunscreen lotion and
sunscreen-containing lip balm should be used daily on the face and lips to
prevent ultraviolet (UV) B-induced outbreaks of HSV. If this does not prevent
recurrences or if genital HSV is the cause, chronic suppressive doses of an
oral antiviral drug for at least 6 months with oral acyclovir
(10 mg/kg/day in divided doses), valacyclovir (500–1000 mg/day, with
dose depending upon frequency of recurrences) or famciclovir (250 mg twice
daily) should be considered. This will prevent recurrences in
up to 90% of HSV-related cases, occasionally the beneficial effect can
continue even after the antiviral drug is discontinued. As a rule, antiviral
therapy has minimal impact if given after the appearance of the acute episode
of EM. It is of interest that some patients who suffer from recurrent erythema
multiforme without overt herpes infection are helped by prophylactic acyclovir,
implying that recurrent herpes infection may nevertheless be responsible.
In patients
whose condition fails to respond adequately to antiviral suppression, dapsone,
cyclosporine, or thalidomide may occasionally be helpful. It should be noted that
most cases of EM minor (HAEM) are self-limited and symptomatic treatment may be
all that is required. Oral antihistamines for 3 or 4 days may
reduce the stinging and burning of the skin. Tetracycline is indicated in EM related to Mycoplasma
pneumoniae.
In extensive
cases of EM minor, systemic steroids have been used, but because they
theoretically may reactivate HSV, they are best given concurrently with an
antiviral drug. The response to systemic corticosteroids is often
disappointing. For patients with widespread EM unresponsive to the above therapies,
management is as for severe drug induced SJS.
When a precipitating factor can be identified
(e.g. HSV or M. pneumoniae), specific therapy should be instituted. In severe
forms of EM with functional impairment, early therapy with systemic
corticosteroids at an initial dosage of prednisone [0.5–1 mg/kg/day for
3-5 days]or pulse methylprednisolone [20 mg/kg/day for 3 days]) should be
considered, despite the absence of controlled studies and the long-existing controversy
regarding increasing the risk of infectious complications.
Regarding oral EM, spontaneous healing can be
slow, up to 2–3 weeks in EM minor and up to 6 weeks in EM major. No specific
treatment is available but supportive care is important; a liquid diet and
intravenous fluid therapy may be necessary. Electrolytes and nutritional
support should be started as soon as possible. Oral hygiene should be improved
with 0.2% aqueous chlorhexidine mouth baths. EM minor often responds to topical “swish and spit” mixtures containing
lidocaine, benadryl, and kaolin. Unresponsive cases may respond to topical corticosteroids, although
systemic corticosteroids may still be required. EM major should be treated with
systemic corticosteroids (prednisolone 0.5–1 mg/kg/day tapered over 7–10 days)
and/or azathioprine or other immunomodulatory drugs.
Administration of topical ophthalmic
preparations should be done in conjunction with an ophthalmologist.