Genital Chlamydia infection
Introduction
Genital
Chlamydia infection is one of the most commonly reported STIs globally. Vertical transmission during childbirth can also occur. It causes inflammation of the genital and rectal mucous
membranes as well as the conjunctiva, but is often asymptomatic. The causative
organism, Chlamydia trachomatis, is an exclusively human, obligate,
intracellular bacterial pathogen with a complex life cycle.
Chlamydia
trachomatis serovars A–C are responsible for
ocular trachoma, which is a major cause of blindness worldwide. Genital Chlamydia
D–K strain infections are considered the world's most common sexually
transmitted bacterial pathogens. Chlamydia trachomatis serovars L1–L3
cause lymphogranuloma venereum (LGV).
Chlamydia causes a number of clinical syndromes including urethritis,
cervicitis, epididymo‐orchitis,
pelvic inflammatory syndrome, seronegative reactive arthritis and ophthalmia neonatorum.
Epidemiology
Incidence
and prevalence
In 2008, the WHO reported a global
incidence of genital chlamydia and gonorrhoea with >100 million cases of
each. However, genital chlamydia is considered to be at least three times more
prevalent than gonorrhoea.
Age
Age is the most significant risk
factor for chlamydia, with the highest rates being found in those under 25
years old and a decreasing prevalence with increasing age.
Sex
Chlamydial
infection in women is 2.5 times more than men.
Associated
diseases
Individuals
diagnosed with an STI are at risk of other coexistent STIs, therefore a sexual
health assessment is warranted.
Predisposing
factors
The main predisposing factor for Chlamydia
infection appears to be an age of less than 25 years. Cervical ectopy, where
there is visible columnar epithelium on the ectocervix, is more common in
younger women and the prevalence of chlamydia is greater in women with ectopy
than without.
Pathology
Sub-acute and chronic asymptomatic
infection is common and the infection can persist for many months or years if
untreated. The frequent absence of symptoms in the acute phase facilitates
spread.
The clinical manifestations of Chlamydia
infection are probably a direct result of tissue damage as well as host immune
response, resulting in scarring of the affected mucous membranes.
Causative
organisms
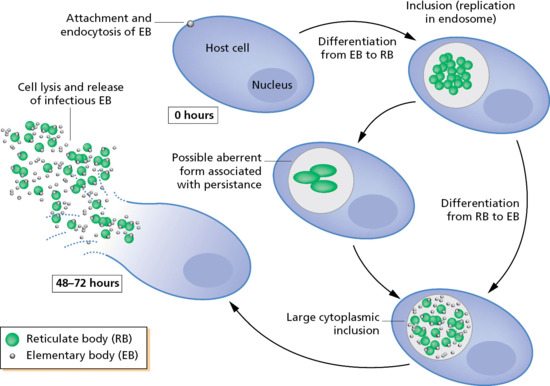
Chlamydiae
are obligate intracellular parasites and exhibit a unique, two‐stage developmental cycle with two
forms:
·
An extracellular, infectious
elementary body (EB).
·
An intracellular, replicative
reticulate body (RB).
This cycle begins when infectious,
metabolically inert EBs attaches to and stimulate uptake by the host cell. The
internalized EB remains within a host‐derived vacuole, termed an inclusion, and differentiate into
a larger, metabolically active RB. The RB multiplies by binary fission, and
after 8–12 rounds of multiplication, the RBs differentiate to EBs asynchronously.
At 48–72 h post‐infection,
EB progeny are released from the host cell to initiate another cycle.
C.
trachomatis strains A–K primarily infect
squamocolumnar epithelial cells.
Clinical
features
Asymptomatic
infection occurs in up to 90% of women and more than 50% of men.
In men, the most common manifestation of disease is anterior
urethritis, characterized by a mucopurulent urethral discharge and dysuria, with an onset 1–3 weeks after
intercourse with an infected partner. Note that the discharge due
to Chlamydia is classically less purulent, less profuse, and less spontaneous
when compared to urethral gonorrhea. Rectal infection may result in proctitis
in men practising receptive anal
intercourse which may be asymptomatic, but some will have symptoms
resembling those seen with gonococcal proctitis. It is important to exclude LGV if rectal symptoms are
present.
In
women, the columnar epithelium of the endocervix is commonly affected. Common
symptoms include inter menstrual or post coital bleeding and vague but persistent
lower abdominal pain, vaginal discharge and dysuria. Typically, in such patients there are signs of mucopurulent
cervicitis and/or contact bleeding.
Extragenital
infections also occur. Pharyngeal infections are usually asymptomatic.
Infection of the eye causes acute follicular conjunctivitis which is usually,
but not always, associated with genital infection. Acute follicular conjunctivitis
is usually associated with Chlamydia whereas chronic conjunctivitis may be seen
in trachoma or lymphogranuloma venereum. Neonates may develop conjunctivitis and
pneumonia after being infected from passage through the birth canal of an
infected mother. Chlamydia in pregnancy may be
associated with premature labor and preterm birth.
Complications and co‐morbidities
Complications mostly occur from
ascending infections and possibly from dissemination, and are also associated
with pregnancy and the neonatal period.
Ascending infection in men causes
epididymo‐orchitis.
Epididymo‐orchitis in
those less than 35 years old is most likely to be caused by a sexually
transmitted organism such as C. trachomatis. Thus, aside from urethral discharge, men
may also present with unilateral scrotal pain and swelling. In those over 35 years old urological pathogens such as Escherichia
coli, Klebsiella sp. or enterococci are more likely.
Chlamydia should be considered as a possible
cause for a Bartholin abscess, with or without concurrent gonococcal infection.
In the absence of treatment, 10–40% of women infected with Chlamydia
will develop PID, with ascending infection to the uterus and
fallopian tubes. Symptoms may include fever, lower abdominal pain, back pain,
vomiting, vaginal bleeding, dyspareunia, and adnexal or cervical motion
tenderness on physical examination. Sequelae of untreated infection include
tubo-ovarian abscesses, ectopic pregnancies, chronic pelvic pain, and
infertility due to chronic inflammation with resultant scarring. The risk of developing PID increases with
each recurrence of C.
trachomatis infection, as does the risk of reproductive
sequelae. Five to ten percent of women with chlamydial PID may develop
perihepatitis. Fitz‐Hugh–Curtis
syndrome presents as upper‐right‐sided abdominal pain and fibrinous
‘violin‐string’ adhesions of the liver capsule as a consequence of
perihepatitis.
Chlamydia
is strongly associated with reactive arthritis and is termed sexually acquired
reactive arthritis (SARA). Reactive arthritis can occur up to 1 month after symptoms
of nongonococcal urethritis (NGU) due to chlamydia. Reactive arthritis can be defined as a sterile inflammatory
arthritis following bacterial infection elsewhere. Individuals with the
haplotype HLA-B27 are at increased risk of developing the reactive arthritis
syndrome. SARA occurs in 0.8–4% of those
infected with Chlamydia. It is a seronegative, asymmetrical,
spondyloarthropathy with or without extra‐articular features that include the following:
·
Mucocutaneous manifestations
including circinate balanitis, erosions affecting the buccal and rectal mucosa
and keratoderma blenorrhagica.
·
Iritis and conjunctivitis.
Prognosis and Clinical
Course
Early treatment with
appropriate antibiotic therapy results in excellent prognosis and reduces the
risk of long-term complications, such as infertility from PID. It is important
to complete an appropriate course of antibiotic.
Laboratory Tests
Traditionally, chlamydial infection was diagnosed by
tissue culture with specimens obtained from the endocervix in women, urethra in
men, and rectum, or conjunctivae, as indicated. More rapid and sensitive tests
have replaced culture in recent years. A direct fluorescent antibody test,
which is highly specific, can be performed on endocervical and penile urethral
specimens with rapid results. Less invasive tests involving nucleic acid
hybridization and nucleic acid amplification, such as PCR, is more commonly
being used to detect even small amounts of chlamydial DNA in urethral, vaginal,
endocervical swabs and in first voided urine samples. It should be noted that
the nucleic acid amplification and hybridization tests are less accurate for
chlamydial detection from rectal and oropharyngeal sites than from genital
sites.
First‐void urine is the sample of choice in men, and in females a
self‐taken vaginal
swab or an endocervical swab are acceptable. In MSM and commercial sex workers,
pharyngeal and rectal testing may also be indicated and NAATs are the only
recommended test. Conjunctival sampling may also be clinically indicated in
some situations.
There
is also some debate about exactly who should receive chalmydial testing, aside
from those whose symptoms suggest that diagnosis. The CDC recommends annual
screening of all sexually active women under the age of 25 and for older women
with risk factors (e.g., those who have a new sex partner or multiple sex partners).
Treatment
Treatment is indicated if chlamydia
is diagnosed or if there is a history of contact with a person known to be
infected. Patients with chlamydia should always be fully assessed and screened
for other STIs and HIV. They should be asked to abstain from sexual contact for
7 days after they and their partners have received treatment and their symptoms
have resolved.
Resistance in C. trachomatis
has been infrequently reported and single‐dose azithromycin is the treatment of choice. It is not
licensed in pregnancy but is recommended by the WHO.
In
complicated infections, more prolonged courses of treatment are employed and
specialist advice may be required.
Uncomplicated
infection
First line
·
Azithromycin 1 g stat (including in
pregnancy)
Second line
·
Doxycycline 100 mg b.d. for 7 days
Third line
·
Ofloxacin 200.300 mg b.d. for 7 days
·
Amoxicillin 500 mg four times a day
for 7 days (pregnancy only)
Complicated
infection
Chlamydial PID
·
Ceftriaxone 500 mg IM single dose+
oral doxycycline 100 mg twice daily and metronidazole 400 mg twice daily for 14
days
Or
·
Ofloxacin 400 mg PO twice daily +
metronidazole 400 mg PO twice daily for 14 days (if gonorrhoea is unlikely)
Epididymo‐orchitis
·
Ceftriaxone 500 mg IM single dose+ doxycycline
100 mg PO twice daily for 10.14 days
Or
·
Ofloxacin 200 mg PO twice daily for
14 days (if gonorrhoea is unlikely)
Chlamydia‐associated
reactive arthritis
·
Rest
·
Non‐steroidal anti‐inflammatory drugs
·
Seek specialist advice