Herpes zoster
Salient features
- Herpes
zoster is characterized by unilateral dermatomal pain and rash that
results from reactivation and multiplication of latent VZV that persisted
within neurons following varicella.
- The
erythematous maculopapular and vesicular lesions of herpes zoster are
clustered within a single dermatome, because VZV reaches the skin via the
sensory nerve from the single ganglion in which latent VZV reactivates,
and not by viremia.
- Herpes
zoster is most common in older adults and in immunocompromised
individuals.
- Pain
is an important manifestation of herpes zoster. The most common
debilitating complication is chronic neuropathic pain that persists long
after the rash resolves, a complication known as postherpetic neuralgia
(PHN).
- Antiviral
therapy and analgesics reduce the acute pain of herpes zoster. Lidocaine
patch (5%), high-dose capsaicin patch, gabapentin, pregabalin, opioids,
and tricyclic antidepressants may reduce the pain of PHN.
- A
live attenuated Oka/Merck strain VZV herpes zoster vaccine (ZVL; Zostavax®)
reduces the incidence of herpes zoster by one-half and the incidence of
PHN by two-thirds. An adjuvanted recombinant glycoprotein E subunit herpes
zoster vaccine (RZV; Shingrix®) has substantially greater
efficacy for herpes zoster and PHN, but it requires 2 doses and is more
reactogenic.
Introduction
Zoster
(zoster = a girdle, a reference to its segmental distribution) affect
individuals who have previously had clinical or subclinical varicella or vaccination. Zoster patients are
infectious, both from virus in the lesions and, in some instances, the
nasopharynx. In susceptible contacts of zoster, chickenpox can occur.
Epidemiology
Although the incidence and severity of herpes
zoster increase substantially in middle to late adulthood, it can occur at any
age and is more common in younger persons who had a varicella infection within
the first year of life. Overall, individuals with a history of varicella have a
20% lifetime chance of developing zoster. Incidence of herpes zoster
is determined by factors that influence the host-virus relationship.
One strong risk
factor is older age. The incidence of zoster increases with age and the mean age of zoster is about 60 years.
Another major risk factor is cellular immune dysfunction.
Immunosuppressed patients have a 20–100 times greater risk of herpes zoster
than immunocompetent individuals of the same age. Immunosuppressive conditions
associated with high risk of herpes zoster include HIV infection, bone marrow
transplant, leukemia and lymphoma, use of cancer chemotherapy, and use of
corticosteroids. Herpes zoster is a prominent and early “opportunistic
infection” in persons infected with HIV, in whom it is often the first sign of
immune deficiency. Thus, HIV infection should be considered in individuals who
develop herpes zoster.
Other factors reported to increase the risk of herpes
zoster include female sex, mental and physical
stress, a family history of zoster, use of tofacitinib or proteasome inhibitors
(e.g. bortezomib, carfilzomib), physical trauma in the affected
dermatome and IL-10 gene polymorphisms.
Virus reactivation usually occurs once in a lifetime. Second
episodes of herpes zoster are uncommon in immunocompetent persons, and third
attacks are very rare. Persons suffering more than one episode may be
immunocompromised. Immunocompetent patients suffering multiple episodes of
herpes zoster-like disease are likely to be suffering from recurrent
zosteriform herpes simplex virus infections.
Patients with herpes zoster are less contagious than
patients with varicella. Virus can be isolated from vesicles and pustules in
uncomplicated herpes zoster for up to 7 days after the appearance of the rash,
and for much longer periods in immunocompromised individuals. Fluid from herpes zoster vesicles can transmit VZV to
seronegative individuals, leading to varicella but not herpes zoster. The
transmission rate to susceptible household contacts is ~15% for zoster,
compared to 80–90% for varicella. Patients with uncomplicated dermatomal
zoster appear to spread the infection via aerosols.
There is evidence that
exposure to
persons with varicella has been reported to increase levels of VZV-CMI and can protect seropositive adults from the development of
zoster. With the universal use of varicella vaccination and decrease in
pediatric and adolescent varicella cases, could
reduce this immune boosting effect, so thatolder persons will no longer
have periodic boosts of the anti-VZV immune activity. This could result in an
increase in the incidence of zoster.
Predisposing
factors
An earlier infection with varicella
is essential before zoster can occur. Most commonly, chickenpox occurs in
childhood and zoster in middle to older age.
Herpes zoster appears upon
reactivation of latent VZV, which may occur spontaneously or induced by other
factors. The mechanisms involved in reactivation of latent VZV are unclear, but
reactivation has been associated with immunosuppression; emotional stress;
irradiation of the spinal column; tumor involvement of the cord, dorsal root
ganglion, or adjacent structures; local trauma; surgical manipulation of the
spine; and frontal sinusitis (as a precipitant of ophthalmic zoster). Most
important, though, is the decline in VZV-specific cellular immunity that occurs
with increasing age.
Pathogenesis
Proposed
pathogenesis of herpes zoster with establishment of persistent but latent
varicella–zoster virus in the sensory-nerve ganglia.
During the course of varicella,
VZV passes from lesions in the skin and mucosal surfaces into the contiguous
endings of sensory nerves and is transported centripetally up the sensory
fibers to the sensory ganglia (the dorsal root ganglia (DRG) of the spinal nerves and the sensory ganglia
of the cranial nerves, also known as cranial nerve ganglia). In the ganglia, the
virus establishes a latent infection where it can remain dormant for several
decades before being reactivated in later life to cause HZ (shingles). The VZV genome persists, both in the neurons and in the glial cells. Despite extensive
research, the molecular and immunological mechanisms responsible for latency
and reactivation are incompletely understood. However, VZV-specific cellular
immunity appears to be critical. Reactivation occurs in those ganglia in which VZV has
achieved the highest density - those innervated by the first (ophthalmic) division of
the trigeminal nerve and by spinal sensory ganglia from T1 to L2.
VZV may also reactivate without producing overt disease.
The small quantity of viral antigens released during such contained
reactivations would be expected to stimulate and sustain host immunity to VZV.
Varicella
and herpes zoster (A) During primary VZII infection (varicella or chicken pox),
virus infects sensory ganglia. (B) VZV persists in a latent phase within
ganglia for the life of the individual. (C) With diminished immune function,
VZV reactivates within sensory ganglia, descends sensory nerves, and replicates
in skin.
When
VZV-specific T cellular immunity falls below some critical level, during ageing
or as a result of immunosuppression, reactivated virus can no longer be contained, virus reactivates from ganglionic neurons
and spreads peripherally or centrally to cause disease. The virus continues
to replicate in the affected ganglion and produces a painful ganglionitis. The reactivation of the VZV destroys a
larger part of the ganglion in the neurons and glial cells. This leads to acute
zoster-associated pain. Infectious virions then spreads antidromically
down the sensory nerve, causing neuronal inflammation and necrosis that can
result in severe neuralgia, and is released from the sensory nerve endings in
the skin/mucosa, where it produces
the characteristic cluster of zoster vesicles. Spread of the ganglionic
infection proximally along the posterior nerve root to the meninges and cord
may result in local leptomeningitis, cerebrospinal fluid pleocytosis, and
segmental myelitis. Infection of motor neurons in the anterior horn and
inflammation of the anterior nerve root account for the local palsies that may
accompany the cutaneous eruption.
Central spread to the brain causes meningoencephalitis, while central spread to
intracranial and extracranial arteries produces vasculopathy and
varicella-zoster virus temporal arteritis, respectively. Viremia also occurs
during herpes zoster.
Pain is a major symptom of herpes zoster. It
often precedes and generally accompanies the rash, and it frequently persists
after the rash has healed—a complication known as postherpetic neuralgia (PHN).
Zoster can cause some destruction of
nerve fibers in the middle and lower dermis that may persist for over a year
and characteristically does so in patients with post‐herpetic
neuralgia. The inflammation in the nerve
tissue can last for a very long time, cause scars, and loss of certain glial
cells (neuronophagy) that triggers a deafferentiation of the sensory ganglion,
which, in turn, triggers postherpetic neuralgia.
Fluctuation of varicella–zoster virus cellular immunity with
age
Varicella
is the primary infection during childhood that
results in an immune response, which leads to VZV-specific cell-mediated
immunity. Resolution of the primary infection results in the induction of
memory T cells specific for VZV, but the frequency of these T cells and
consequent cellular immunity declines over time. However, it can be enhanced
during an individual's lifetime by two processes:
·
Exogenous boosting as
a result of being in contact with individuals with varicella (chickenpox)
·
Endogenous boosting
as a result of subclinical reactivation of latent virus residing within the
ganglia
Clinical Manifestation
Herpes
zoster classically occurs unilaterally within the distribution of a cranial or
spinal sensory nerve, often with some overflow into the dermatomes above and
below. Rarely, the eruption may be
bilateral.
The
most commonly affected dermatomes are the second cervical to second lumbar
nerves (C2 to L2) and the fifth and seventh cranial nerves.
The thoracic (53%), cervical
(usually C2,3,4, 20%), trigeminal, including ophthalmic (15%), lumber (13%) and
sacral (2%) dermatomes are most commonly involved at all ages, but the relative
frequency of ophthalmic zoster increases in old age. Possibly because
chickenpox is centripetal (located on the trunk), the thoracic region is
affected in two thirds of herpes zoster cases. Herpes zoster manifests in three distinct clinical
stages: (1) prodrome, (2) Eruptive phase, and (3) PHN.
Prodrome of Herpes Zoster
Pain and paresthesia (tingling, burning) in the involved dermatome often precede the
eruption by 1-5 days and persists for 2–3 weeks
(84% of cases). The
pain may become quite intense, constant or intermittent and it is often
accompanied by fever, headache, malaise and tenderness localized to areas of one or more dorsal roots and hyperesthesia of
the skin in the involved dermatome.
The pain may be sharply localized and unilateral, but may be more diffuse. This pre-eruptive
pain of herpes zoster may lead to serious misdiagnosis and misdirected
interventions. There is a correlation with the pain severity and extent of the skin
lesions. Prodromal pain is minimal in immunocompetent persons under 30 years of
age, but it more severe in persons over the age of 60 years. Instead of or in addition to pain, occasionally pruritus may
be an early feature of shingles. The time between the start of the pain and the
onset of the eruption is much less in trigeminal zoster than in thoracic
disease.
A
few patients experience acute segmental neuralgia without ever developing a
cutaneous eruption—a condition known as zoster sine herpete.
Eruptive
phase
Within
1-5 days of the onset of pain, cutaneous lesions appear. Pain, paresthesia and
hyperesthesia can be present.
The most distinctive feature of herpes
zoster is the localization and distribution of the rash, which is nearly always
unilateral and is generally limited to the area of skin innervated by a single
sensory ganglion. The area supplied by the trigeminal nerve, particularly the
ophthalmic division, and the trunk from T3 to L2 are most frequently affected;
lesions rarely occur distal to the elbows or knees.
Although the individual lesions of herpes zoster and
varicella are indistinguishable, those of herpes zoster tend to evolve more
slowly and usually consist of closely grouped vesicles on an erythematous base,
rather than the more discrete, randomly distributed vesicles of varicella. This
difference reflects intraneural spread of virus to the skin in herpes zoster,
as opposed to viremic spread in varicella.
Classically, HZ is a unilateral, dermatomal eruption,
with skin lesions evolving simultaneously from erythematous macules to papules,
vesicles, pustules, and final crusting. Usually not the entire dermatome is
involved. Herpes zoster lesions begin as closely
grouped red papules, rapidly becoming vesicles on an erythematous,
edematous base within 12–24 hours, which may be umbilicated and then pustular by the third day. There may be
bullae formation also. A dusky purple color may
be observed in older vesicles. These dry and crust in 7–10 days. The
adherent crust generally persists for 2–4 weeks and then heals with scarring. In
some cases vesicles do not form or are so small that they are difficult to see.
The vesicles vary in size, in contrast to the cluster of uniformly sized
vesicles noted in herpes simplex. The lesions develop in a continuous or interrupted band in the area of
one, occasionally two and, rarely, three contiguous dermatomes. It
is not uncommon for there to be scattered lesions outside the dermatome,
usually fewer than 20. In normal individuals, new lesions
continue to appear for up to 1 week. The
striking feature is cut‐off
at the mid line, except that a few lesions may appear just
over the line, reflecting the paths of small nerve branches. Often in children, and occasionally
in adults, the eruption is the first indication of the attack. The
rash is most severe and lasts longest in older people, and is least severe and
of shortest duration in children.
Lesions may develop on the mucous
membranes within the mouth in zoster of the maxillary or mandibular division of
the facial nerve, or in the vagina in zoster in the S2 or S3 dermatome.
Regional
nodes draining the area are often enlarged and tender.
Clinical
variants
TRIGEMINAL NERVE
ZOSTER
The fifth cranial, or trigeminal,
nerve has three divisions: the ophthalmic, maxillary, and mandibular. The
ophthalmic division further divides into three main branches: the frontal,
lacrimal, and nasociliary nerves. Involvement of any branch of the ophthalmic
nerve is called herpes zoster ophthalmicus. It constitutes 10% to 15% of all
zoster cases. Involvement of the ophthalmic branch of the fifth cranial nerve
is five times as common as involvement of the maxillary or mandibular branches.
Ophthalmic
zoster
In herpes zoster ophthalmicus (HZO),
the ophthalmic division of the fifth cranial nerve is involved. This ophthalmic
branch sends branches to the tentorium and to the third and sixth cranial
nerves, which may explain the meningeal signs and, occasionally, the third and
sixth cranial palsies associated with herpes zoster ophthalmicus. Ipsilateral rash extends from eye level to the
vertex of the skull but does not cross the midline.
Ipsilateral preauricular
and, occasionally, submaxillary nodal involvement is a common prodromal event
in HZO and often is valued equivalently with pain, vesiculation, and erythema
in establishing a diagnosis. Prodromal lymphadenopathy should not be confused
with the later reactive adenopathy caused by secondary infection of vesicles.
Headaches, nausea, and vomiting also are common prodromal symptoms.
Herpes zoster ophthalmicus may be
confined to certain branches of the trigeminal nerve. If the external division
of the nasociliary branch is affected, which supplies the nasal tip, dorsum and
root of the nose and the medial canthus as well as the cornea, with vesicles on
the side and tip of the nose (Hutchinson’s sign), the eye is involved 76% of
the time, as compared with 34% when it is not involved. Vesicles on the lid
margin are virtually always associated with ocular involvement. In any case,
the patient with ophthalmic zoster should be seen by an ophthalmologist.
Aggressive
treatment with systemic
antiviral therapy should be started immediately, pending ophthalmologic
evaluation. ~50% of patients have ocular involvement, which can include
conjunctivitis, (epi)scleritis, keratitis, uveitis, acute retinal necrosis, and
optic neuritis. May lead to ocular scarring and visual loss. These
complications are reduced from 50% of patients with herpes zoster ophthalmicus
to 20–30% with effective antiviral therapy.
In the absence of prompt
detection and treatment, eye involvement poses a risk to vision. The presence
of orbital edema is an ophthalmologic emergency, and patients must be referred
immediately for specialized ophthalmic evaluation and treatment. Involvement of
the area below the palpebral fissure alone, without upper eyelid or nasal
involvement, is considered less likely to result in ocular complications, in
that the superior maxillary nerve innervates the lower eyelid.
Unlike the cutaneous
lesions, ocular lesions of zoster and their complications tend to recur,
sometimes as long as 10 years after the zoster episode.
Since (intra) ocular
involvement is common and may not be noted by general inspection,
ophthalmologist advice should be recommended in the event of facial HZ with
ocular involvement, in order to determine the treatment strategy and necessity
for ophthalmologist reassessment. The most accurate method to confirm the
diagnosis of intraocular involvement is to demonstrate the presence of VZV DNA
or intraocular production of anti-VZV antibodies.
Postherpetic complications are
more common in HZO than in other manifestations of zoster. In
particular, PHN is observed in well over 50% of patients with HZO and can be
severe and long-lasting. Scarring also is more common, probably as a result of
severe destructive inflammation.
Involvement
of the other sensory branches of the trigeminal nerve is most likely to yield
periocular involvement but spare the eyeball. Involvement
of the ciliary ganglia may give rise to Argyll–Robertson pupil.
Herpes zoster of maxillary branch of
cranial nerve(CN) V
Involvement of CN V2 is
localized to the ipsilateral cheek, the lower eyelid, the side of the nose, the
upper eyelid, the upper teeth, the mucous membrane of the nose, the
nasopharynx, on one side of the palate, uvula and
tonsillar area, the upper gingiva and buccal sulcus. At
times, only the oral mucous membrane is involved, and there are no cutaneous
manifestations. Herpes zoster of the maxillary division of the trigeminal nerve
may begin with toothache during its prodromal stage, followed by its vesicular
eruption. So this preeruptive herpetic pain may result in
unnecessary oral surgery or dental treatment.
Herpes zoster of mandibular branch
of CN V
Areas of CN V3 involvement
include vesicles
appear on one side of the head, the external ear
and external auditory canal, one side of the tongue, the floor of the
mouth, lower labial and buccal mucosa. As when
other branches of CN V are involved, prodromal pain in affected areas can
result in incorrect diagnoses.
Herpes
zoster oticus
The facial nerve, mainly a motor
nerve, has vestigial sensory fibers supplying the external ear (including pinna
and meatus) and the tonsillar fossa and adjacent soft palate. Classical sensory
nerve zoster in these fibers causes pain and vesicles in part or all of that
distribution.
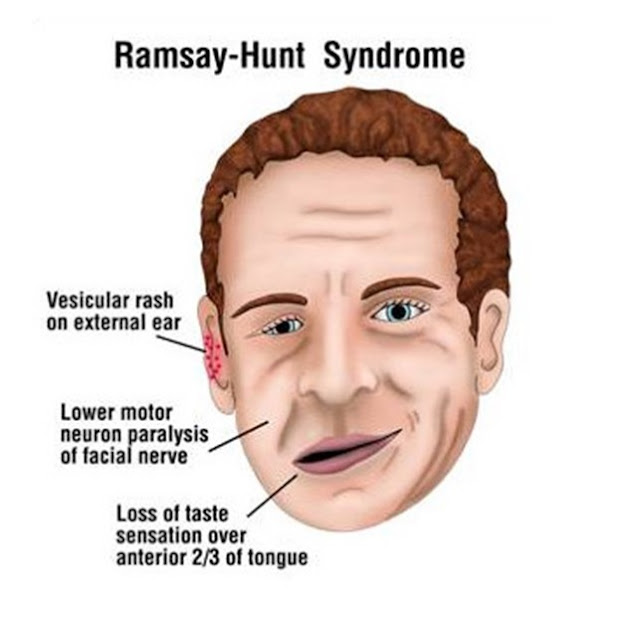
Ramsay
Hunt syndrome results from involvement of the facial and auditory nerves by
VSV. Herpetic inflammation of the geniculate ganglion is felt to be the cause
of this syndrome.
There
is involvement of the sensory portion and motor portion of the seventh cranial
nerve. There may be unilateral loss of taste on the anterior two thirds of the
tongue as well as vesicles on the tympanic membrane, external auditory meatus,
concha, and pinna, tonsillar fossa and adjacent soft
palate.
Involvement of the motor division of the seventh cranial nerve causes
unilateral facial paralysis. If the vestibulocochlear nerve is also affected
due to the close proximity of the geniculate ganglion to the vestibulocochlear
nerve within the bony facial canal: tinnitus, vertigo, otalgia, nausea,
vomiting, nystagmus and deafness.
It is recommended to seek advice of an
otorhinolaryngologist, especially in the case of involvement of the facial or
auditory nerves, in order to determine the treatment strategy and necessity for
otorhinolaryngologist reassessment.
Sacral zoster (S2, S3,
or S4 dermatomes)
A
neurogenic bladder with urinary hesitancy or urinary retention has reportedly
been associated with zoster of the sacral dermatome S2, S3, or S4. Migration of
virus to the adjacent autonomic nerves is responsible for these symptoms.
Herpes zoster sine
herpete
It is defined as the presence of unilateral dermatomal
pain without cutaneous lesions in patients with virologic and/or serologic
evidence of VZV infection. The most accurate method to confirm the diagnosis is
to demonstrate an increase in the blood of anti-VZV IgG and IgM. The
identification of specific serum IgA may be of additional value. In cases of HZ
sine herpete with facial palsy, VZVDNA may be detected in oropharyngeal swabs
2–4 days after the onset of facial palsy using PCR.
Childhood HZ is
quite similar to adult HZ, but ZAP is absent in the majority of cases.
Pain of acute Herpes Zoster
Although the rash is
important, pain is the cardinal problem of acute herpes zoster, especially in
the elderly. Most patients experience dermatomal pain or discomfort during the
acute phase (The first 30 days following rash onset) that ranges from mild to
severe. Patients describe their pain or discomfort as burning, deep aching,
tingling, itching, or stabbing. For some patients, the pain intensity is so
great that words like horrible or excruciating are used to describe the
experience.
Herpes zoster during pregnancy
Herpes zoster during pregnancy,
whether it occurs early or late in the pregnancy, appears to have no
deleterious effects on either the mother or the infant.
Herpes Zoster in the Immunocompromised Host
Except for PHN, most serious complications of herpes
zoster occur in immunocompromised persons. In
immunocompromised patients, both the incidence and severity of zoster are
increased, and it is frequently complicated by generalized varicella
(‘disseminated zoster’). Cutaneous dissemination is defined
as more than 20 vesicles outside the area of primary or adjacent dermatomes producing
a varicella-like eruption and is probably a result of hematogenous spread of
the virus. The dermatomal lesions are sometimes hemorrhagic or gangrenous. The
outlying vesicles or bullae, which are usually not grouped, resemble varicella
and are often umbilicated and may be hemorrhagic. This is seen in malignancy, especially
lymphomas, AIDS and also in patients receiving immunosuppressive therapy. If
the rash spreads widely from a small, painless area of herpes zoster, the
initial dermatomal presentation may go unnoticed, and the ensuing disseminated
eruption may be mistaken for varicella. Patients with cutaneous dissemination
also manifest widespread, often fatal, visceral dissemination, particularly to
the lungs, liver, and brain that occurs in 10% of
immunocompromised patients. Anti‐tumour necrosis factor (TNF) ‐α therapy is estimated to increase
the risk of zoster threefold.
In
patients infected with HIV, zoster is 10 times more common than in the normal
population and
may be the earliest clinical sign of the development of AIDS in high-risk
individuals. HIV-infected patients are fairly unique in their tendency to
suffer multiple recurrences of herpes zoster as their HIV infection progresses;
herpes zoster may recur in the same or different dermatomes or in several
contiguous or noncontiguous dermatomes. Herpes zoster in patients with AIDS may
be severe, with cutaneous and visceral dissemination. Patients with AIDS may
also develop chronic verrucous, hyperkeratotic, or ecthymatous cutaneous
lesions caused by acyclovir-resistant VZV.
Unilateral herpes zoster involving
multiple dermatomes
Involvement of more than 1
dermatomal distribution in unilateral zoster is rare and usually is considered
a harbinger of significant compromise of the immune system caused by AIDS,
malignancy, chemotherapy, and other factors. Involvement of 2 dermatomes may be
referred to as zoster duplex, and involvement of 3 or more may be referred to
as zoster multiplex.
Bilateral herpes zoster
On rare occasions, herpes
zoster manifests bilaterally. Bilateral presentations should always raise
concern for disseminated disease (and immunocompromise) or for alternate
diagnosis, specifically for herpes simplex.
In cases of bilateral zoster,
it is not unusual for 1 or 2 adjacent dermatomes to be involved. Unlike
examples of multiple dermatomal involvements in unilateral disease, involvement
in adjacent dermatomes is not typically a sign of underlying disease (eg,
malignancy).
Recurrent herpes zoster
Recurrences of herpes zoster do
occur rarely and are not limited to those who are immunocompromised. The
incidence rate of herpes zoster is 5.1 cases per 1000 person years; its
recurrence rate was calculated at 12 cases per 1000 person years. Risk factors
include old age (51-70 years) and zoster-related pain longer than 30 days. Many
cases of recurrent zoster involve other entities, usually herpes simplex in a
linear distribution.
Complications
and co‐morbidities
Complications of Herpes Zoster
|
Cutaneous |
Visceral |
Neurologic |
|
Bacterial superinfection |
Pneumonitis |
Postherpetic neuralgia |
|
Scarring |
Hepatitis |
Meningoencephalitis |
|
Zoster gangrenosum |
Esophagitis |
Transverse myelitis |
|
Cutaneous dissemination |
Gastritis |
Peripheral nerve palsies |
|
Pericarditis |
Motor |
|
|
Cystitis |
Autonomic |
|
|
Arthritis |
Cranial nerve palsies |
|
|
Sensory loss |
||
|
Deafness |
||
|
Ocular complications |
||
|
Granulomatous angiitis (causing contralateral
hemiparesis) |
The sequelae of herpes zoster include cutaneous, ocular,
neurologic, and visceral complications. Most complications of herpes zoster are
associated with the spread of VZV from the initially involved sensory ganglion,
nerve, or skin, either via the bloodstream or by direct neural extension. The
rash may disseminate after the initial dermatomal eruption has become apparent.
When immunocompetent patients are carefully examined, it is not uncommon to
have at least a few vesicles in areas distant from the involved and immediately
adjacent dermatomes. The disseminated lesions usually appear within a week of
the onset of the segmental eruption and, if few in number, are easily overlooked.
More extensive dissemination occurs in immunocompromised patients.
When the dermatomal rash is
particularly extensive, as it often is in severely immunocompromised patients,
there may be superficial gangrene with delayed healing and subsequent scarring
which is sometimes hypertrophic or keloidal. Secondary bacterial infection may
also delay healing and cause scarring.
Zoster-associated pain and Post‐herpetic neuralgia
Pain is the most troublesome symptom of zoster. 84% of patients
over the age of 50 will have pain preceding the eruption and 89% will have pain
with the eruption. Various terminologies are used to classify the pain. The
simplest approach is to term all pain occurring immediately preceding or after
zoster “zoster associated pain” (ZAP). Zoster-associated pain includes the entire
pain spectrum of HZ with three distinguishable phases: acute pain phase (up to
first 30 days), subacute pain phase (30–90 days after rash healing) and post
herpetic neuralgia (PHN, pain for more than 90 days after the onset of rash). A
prodromal phase as part of acute ZAP, with an onset of pain or dysaesthesia
prior to visible symptoms of HZ, may additionally be distinguished. In the
prodromal phase of HZ, pain can be observed 2–18 days before the appearance of
skin lesions, often leading to a wide array of erroneous diagnoses, according
to the anatomical site of VZV reactivation, including myocardial infarction,
cholecystitis, etc.
PHN is the commonest and
most intractable sequel of zoster, and its incidence increases with
increasing age. It may develop as a continuation of
the pain that accompanies acute zoster, or it may develop after apparent
resolution of the initial zoster reactivation and generally defined as persistence or recurrence of pain more
than a month after the onset of zoster, but better considered after 3 months. The
pain may last for months to years.
Age is the most significant risk factor for PHN. The
tendency to have persistent pain is age dependent, occurring for longer than 1
month in only 2% of persons under 40 years of age. 50% of persons over 60 years
of age and 75% of those over 70 years of age continue to have pain beyond 1
month. Although the natural history is for gradual improvement in persons over
70 years, 25% have some pain at 3 months and 10% have pain at 1 year. Severe
pain lasting longer than 1 year is uncommon, but 8% of persons over 60 have
mild pain and 2% still have moderate pain at 1 year. Individuals affected by
ophthalmic HZ with keratitis or intraocular inflammation are found to be at
higher risk for PHN. A scoring system for the calculation of the individual PHN
risk, including the following risk factors has been proposed: female gender,
age >50 years, the presence of prolonged
prodromal
pain, severe pain during the acute phase of herpes zoster, prolonged
with greater rash severity with >50 lesions, more extensive sensory
abnormalities in the affected dermatome, cranial/sacral localization, and
hemorrhagic lesions. In the majority of
cases, PHN progressively improves and after 1 year only 1–2% of the patients
still experience pain.
The quality of pain associated with herpes zoster varies,
but three basic types of pain have been
described: the constant, monotonous pain (described as
“burning, deep aching, or throbbing”), intermittent pain (“stabbing, shooting”,
lancinating (neuritic)), and/or stimulus-evoked pain. The latter is usually
allodynia (pain with normal nonpainful stimuli such as light touch) or
hyperalgesia (severe pain produced by a stimulus normally producing mild pain).
Allodynia is a particularly disabling component of the disease that is present
in approximately 90% of patients with PHN. Patients with allodynia may suffer
severe pain after even the lightest touch of the affected skin by things as
trivial as a breeze or a piece of clothing. These subtypes of pain may produce
disordered sleep, depression, anorexia, weight loss, chronic fatigue, and
social isolation, and they often interfere with dressing, bathing, general
activity, traveling, shopping, cooking, and housework. The character and
quality of acute zoster pain are identical to the pain that persists after the
skin lesions have healed, although they are mediated by different mechanisms.
Herpes zoster can be
more severe and extensive, with disseminated and/or confluent involvement of
the skin. Patients at risk of severe HZ and hence at increased risk for
cutaneous and/or systemic dissemination as well as more severe PHN can be
identified by a series of risk factors, such as age older than 50 years,
moderate to severe prodromal or acute pain, immunosuppression including cancer,
haemopathies, HIV infected, solid organ and bone marrow transplant recipients,
and other patients receiving immunosuppressive therapies. Certain clinical
findings at an early stage of HZ identify patients at higher risk of
complications. These include the presence of satellite lesions (aberrant
vesicles), severe rash and/or involvement of multiple dermatomes or
multi segmental HZ, simultaneous presence of lesions in different developmental
stages, altered general status, and meningeal or other neurological signs and
symptoms. So it is recommended to search for these signs in patients presenting
with HZ.
Disease
course and prognosis
The total duration of the eruption depends on
three factors: patient age, severity of eruption, and presence of underlying
immunosuppression. The pain and the constitutional symptoms subside gradually
as the eruption disappears. In uncomplicated cases recovery is complete in 2–3
weeks in children and young adults, and 3–4 weeks in older patients. The elderly or
debilitated patients may have a prolonged and difficult course. For these
patient populations, the eruption is typically more extensive and inflammatory,
occasionally resulting in hemorrhagic blisters, skin necrosis, secondary
bacterial infection, or extensive scarring, which is sometimes hypertrophic or
keloidal.
Diagnosis of Herpes
Zoster
In the preeruptive stage, the prodromal pain of herpes
zoster is often confused with other causes of localized pain. Once the eruption
appears, the character and dermatomal location of the rash, coupled with
dermatomal pain or other sensory abnormalities, usually makes the diagnosis
obvious.
A cluster of vesicles, particularly near the mouth or
genitals, may represent herpes zoster, but it may also be recurrent HSV
infection. Zosteriform herpes simplex is often impossible to distinguish from
herpes zoster on clinical grounds. A history of multiple recurrences at the
same site is common in herpes simplex but does not occur in herpes zoster in
the absence of profound and clinically obvious immune deficiency.
Where the diagnosis is uncertain,
confirmation is made by culture or PCR as in chickenpox.
Treatment of Herpes
Zoster
Shingles is a self‐limiting
infection but it is painful, and carries a risk of secondary infection and post‐herpetic neuralgia. Middle-aged and elderly patients with
herpes zoster are urged to restrict their physical activities or even stay home
in bed for a few days. Bed rest may be of paramount importance in the
prevention of neuralgia. Younger patients may usually continue with their
customary activities.
Rest and analgesics are sufficient
for mild attacks of zoster in the young. Higher strength analgesia is often
needed in older patients. Soothing topical preparations with dressings as
blisters break can relieve discomfort. Simple local application of gentle
pressure with the hand or with an abdominal binder often gives great relief of
pain.
Topical Therapy
During the acute
phase of herpes zoster, the application of cool compresses, calamine lotion,
cornstarch, or baking soda may help to
alleviate local symptoms and hasten the drying of vesicular lesions. Cool tap water can be used in a wet compress. The
compresses, applied for 20 minutes several times a day, macerate the vesicles,
remove serum and crust, and suppress bacterial growth. A whirlpool with
Betadine (povidone-iodine) solution is particularly helpful in removing the
crust and serum that occur with extensive eruptions in the elderly. Occlusive
ointments should be avoided, and creams or lotions containing glucocorticoids
should not be used. Bacterial superinfection of local lesions is uncommon and
should be treated with warm soaks; bacterial cellulitis requires systemic
antibiotic therapy. Topical treatment with antiviral agents is not effective.
Antiviral Therapy
Antiviral therapy is the cornerstone in the management of
herpes zoster. The major goals of therapy in patients with herpes zoster are to
(1) limit the extent, duration, and severity of pain and rash in the primary
dermatome; (2) prevent disease elsewhere; and (3) prevent PHN.
Indications for Antiviral
Treatment in Patients with Herpes Zoster
1.
Age
≥50 years
2.
Moderate
or severe pain
3.
Severe
rash
4.
Facial
zoster
5.
Other
complications of herpes zoster
6.
Immunocompromised
state
Normal Patients
Treatment
should be started as early as possible, preferably within 72
hours of the development of skin lesions is optimal, but initiation up to 7
days after onset also appears to be beneficial. The virus is less sensitive to aciclovir in vitro
than HSV and higher doses are recommended. Acyclovir 800 mg five times a day, valaciclovir
1 g or famciclovir 500 mg three times a day for 7 days are
all FDA-approved for the treatment of herpes zoster in immunocompetent
individuals. Treatment leads to more rapid resolution of the skin lesions and,
most importantly, substantially decreases the severity and duration of zoster-associated
pain. Valacyclovir and famciclovir are
as effective as or superior to acyclovir, probably because of better absorption
and higher and more reliable blood levels of antiviral activity are achieved.
They are as safe as acyclovir. If not contraindicated, they are preferable to
acyclovir for oral treatment of herpes zoster. Side- by- side trials have
demonstrated valacyclovir and famciclovir to be of similar efficacy, but one
study from japan showed famciclovir to result in more rapid reduction in acute
zoster pain.
Valacyclovir and famciclovir must be dose adjusted in
patients with renal impairment. In an elderly patient, if the renal status is
unknown, these agents may be started at twice a day dosing (which is almost as
effective), pending evaluation of renal function, or acyclovir can be used. For
patients with renal failure (creatinine clearance of less than 25 mL/min),
acyclovir is preferable.
There
is debate regarding the effect of antiviral treatment in reducing the risk of post‐herpetic neuralgia. In immunocompetent individuals >50 years
of age with acute herpes zoster, famciclovir and valacyclovir are equally
effective (and similar or superior to acyclovir) at reducing the frequency and
duration of postherpetic neuralgia if
started early in shingles.
Because of the lower
risk of PHN, antiviral therapy is less valuable or necessary for treatment of
uncomplicated herpes zoster in healthy people younger than 50 years of age. The
utility of antiviral agents is unproven if treatment is initiated more than 72
hours after rash onset. Nevertheless, it is prudent to initiate antiviral
therapy even if more than 72 hours have elapsed after rash onset in patients
who have herpes zoster involving cranial nerves (e.g., ophthalmic zoster) or
who continue to have new vesicle formation.
Antiviral Treatment of Herpes Zoster in the Normal and
Immunocompromised Host
|
Patient Group |
Regimen |
|
Normal |
|
|
Age <50 years |
Symptomatic treatment alone, or Famciclovir
500 mg PO every 8 h for 7 days or Valacyclovir 1
g PO every 8 h for 7 days or Acyclovir
800 mg PO 5 times a day for 7 days a |
|
Age ≥50 years, and patients of any age with cranial
nerve involvement (e.g., ophthalmic zoster) |
Famciclovir
500 mg PO every 8 h for 7 days or Valacyclovir 1
g PO every 8 h for 7 days of Acyclovir
800 –mg PO 5 times a day for 7 days* |
|
Immunocompromised |
|
|
Mild compromise, including HIV-1 infection |
Famciclovir
500 mg PO every 8 h for 7–10 days or Valacyclovir 1
g PO every 8 h for 7–10 days or Acyclovir
800 mg PO 5 times a day for 7–10 days* |
|
Severe compromise |
Acyclovir
10 mg/kg IV every 8 h for 7–10 days |
|
Acyclovir resistant (e.g., advanced AIDS) |
Foscarnet
40 mg/kg IV every 8 h until healed |
* Famciclovir
or valacyclovir
are preferred because their greater and more reliable oral bioavailability
result in higher blood levels of antiviral activity, the lower susceptibility
of VZV (compared to HSV), and the existence of barriers to the entry of
antiviral agents into tissues that are sites of VZV replication.
Immunocompromised
Patients
In the
immunosuppressed patient, an antiviral agent should always be given because of
the increased risk of dissemination and zoster associated complications. In
patients with mild immunocompromise and localized herpes zoster, oral
acyclovir, valacyclovir, or famciclovir will usually suffice.
In severe immunocompromised
patients as well as those with ophthalmic zoster, disseminated zoster, or
Ramsay Hunt syndrome, and in patients failing oral therapy, intravenous
acyclovir should be used at a dose of 10 mg/kg 8‐hourly, adjusted for
renal function. Courses of 5, 7 and 10 days have been used and some advocate a
change from intravenous to oral drug after 48 h. Acyclovir accelerated the rate
of clearance of virus from vesicles and halted progression of the disease and
markedly reduced the incidence of visceral and progressive cutaneous
dissemination.
Treating acute zoster pain
Greater
severity of acute pain is a risk factor for PHN, and acute pain may contribute
to central sensitization and the genesis of chronic pain. Therefore, aggressive
pain control is both reasonable and humane. The choice, dosage, and schedule of
drugs are governed by the patient's pain severity, underlying conditions, and
response to specific drugs. Nonsteroidal anti-inflammatory drugs or
acetaminophen treat mild pain. Opioids, such as tramadol, treat moderate to
severe pain. Add gabapentin if needed. Tricyclic antidepressants can be used
when opioids are insufficient. If pain control remains inadequate, regional or
local anesthetic nerve blocks should be considered for acute pain control.
Treatment of Postherpetic Neuralgia
Once
established, PHN is difficult to treat. Despite the vast array of medication
options, PHN is commonly difficult to treat for two reasons. The recommended
medications are simply often not effective. Second, in the elderly who are most
severely affected by PHN, these medications have significant and often
intolerable side effects, limiting the dose one can prescribe. If multiple
agents are combined to reduce the toxicity of any one agent, the side effects
of these agents overlap (sedation, depression, and constipation) and there may
be drug–drug interactions, limiting combination treatment options. Fortunately,
it resolves spontaneously in most patients, although this often requires
several months.
The
following drugs are effective for pain relief in PHN: gabapentin, pregabalin, tricyclic
antidepressants (TCAs), tramadol, lidocaine patch 5%, and
high-concentration 8% capsaicin patch. The choice of
these medications should be guided by the adverse event profiles, potential for
drug interactions, and patient comorbidities and treatment preferences.
Topical Therapy
Topical anesthesia delivered by means of a 5% lidocaine
patch has been shown to produce significant pain relief in patients with PHN.
The 10 × 14-cm lidocaine patch contains 5% lidocaine base, adhesive, and other
ingredients on a polyester backing. It is easy to use and is not associated
with systemic lidocaine toxicity. Up to three patches are applied over the
affected area for 12 hours a day. The disadvantages of the patch are
application site reactions, such as skin redness or rash, and substantial cost.
Eutectic mixture of local anesthetics (EMLA) cream applied once a day over the
affected area under an occlusive dressing is an alternative method of
delivering topical anesthesia.
A single 1-hour application of a high-concentration capsaicin
patch (8%) significantly reduces pain from PHN from the second week after the
capsaicin application throughout a subsequent 12-week period. The high-concentration
patch is generally well tolerated. Adverse events include increases in pain
associated with patch application (usually transient) and application-site
reactions (e.g., erythema). The role of the high-concentration capsaicin patch
in the treatment of PHN is yet to be clearly established, partly because its
long-term benefits are not yet known. However, this intervention has promise
because a single 1-hour application may yield several weeks of pain reduction.
Oral Agents
Three classes of oral medication are used as standards to
manage PHN—tricyclic antidepressants (TCAs), antiseizure medications, and long
acting opiates.
Opiate analgesics
If opiate analgesia is required, it should be provided by
a long acting agent, and the duration of treatment should be limited and the
patient transitioned to another class of agent. Constipation is a major side
effect in the elderly. During painful zoster these patients ingest less fluid
and fiber, enhancing the constipating effects of the opiates. Bulk laxatives
should be recommended. Tramadol is an option for acute pain control, but drug
interactions with the TCAs must be monitored.
Controlled-release oxycodone (10
mg every 12 hours) is an effective analgesic for the management of steady pain,
paroxysmal spontaneous pain, and allodynia. The dose is increased weekly up to
a maximum of 30 mg every 12 hours. Others have found narcotics ineffective for
the long-term control of pain from PHN and to be associated with unacceptable
side effects. The most common side effects are constipation, nausea, and
sedation.
Gabapentin and Pregabalin
These
anticonvulsant drugs are effective in the treatment of pain and sleep
interference associated with PHN. They are FDA approved for the treatment of
post herpetic neuralgia. Mood and quality of life also improve.
Gabapentin has been shown to
produce moderate or greater pain relief in patients with PHN. Gabapentin is
started as a single 300-mg dose on day #1, 600 mg/day on day 2 (two 300-mg
doses), and 900 mg/day on day 3 (three 300-mg doses). The dose can
subsequently be titrated up as needed for pain relief to a daily dose of 1800
mg (three 600-mg doses per day). A minimum of total dose of 600 mg or more is
needed to obtain optimal benefit.
Additional benefit of using doses greater than 1800 mg/day has not
demonstrated. Frequent adverse effects of gabapentin include somnolence,
dizziness, and peripheral edema.
Pregabalin has been shown to
produce 50% or greater pain relief in 50% of patients with PHN. Pregabalin has
improved pharmacokinetics and is dosed at 300 mg or 600 mg daily, depending on
renal function, with better absorption and steadier blood levels. It is
administered in two or three divided doses per day. Begin dosing at 150 mg/day;
dosing may be increased to 300 mg/day within 1 week. Maximum dose is 600
mg/day. Dizziness, somnolence, and peripheral edema are also the most common
adverse effects reported for pregabalin. Pregabalin has a less complicated dose
titration schedule and a faster onset of action than gabapentin.
Tricyclic antidepressants
Low-dose tricyclic antidepressants have
demonstrated considerable efficacy and appear to act by a mechanism independent
from their antidepressant effects (because relief of PHN
occurs at less than antidepressant dosages).
They are particularly useful for patients with hyperesthesia and
constant burning pain. Nortriptyline and
desipramine are
preferred alternatives to amitriptyline
because they cause fewer cardiac adverse effects, sedation, cognitive
impairment, orthostatic hypotension, and constipation in the elderly.
Nortriptyline is a noradrenergic metabolite of amitriptyline. Pain relief occurs
without an antidepressant effect with nortriptyline, and there are fewer side
effects with nortriptyline. Therefore nortriptyline is the preferred
antidepressant, although desipramine may be used if the patient experiences
unacceptable sedation from nortriptyline. For best results, nortriptyline
should be given early in a dose of 25 mg daily and continued for 3–6 months.
These adrenergically active antidepressants may be most effective
if antiviral treatment is given during the acute attack of shingles.
Side effects
include confusion, urinary retention, postural hypotension, and arrhythmias.
Dry mouth occurs in up to 25% of patients with nortriptyline. Constipation,
sweating, dizziness, disturbed vision, and drowsiness occur in up to 15% of
patients with nortriptyline. Use tricyclic antidepressants with caution in
patients with cardiovascular disease, glaucoma, urinary retention, and
autonomic neuropathy. Screen patients older than age 40 for cardiac conduction
abnormalities.
Combination therapy with gabapentin and nortriptyline
produces greater pain relief than either agent alone. The most common adverse
event is dry mouth secondary to nortriptyline. These results suggest that
combination therapy may benefit some individuals with PHN who have responded to
one of the agents chosen, but at the risk of increased adverse effects than
with either drug alone.
If the patient
fails to respond to local measures, oral analgesics, including opiates, TCAs,
gabapentin and pregabalin, referral to a pain center is recommended.
Emotional support
Patients
with PHN can be miserable for several months. Emotional support is another important
therapeutic measure.
Therapeutic ladder of herpes zoster
First line
·
Aciclovir
·
Valaciclovir
·
Famciclovir
Second line
·
Aciclovir, iv
Third line
·
For post‐herpetic neuralgia:
·
Nortriptyline
·
Desipramine
·
Gabapentin
·
Pregabalin
Medications
Commonly Used for Treatment of Pain Associated with PHN
|
Medication |
Dose |
Dose
adjustment |
Maximum
dose |
Side
effects |
|
OPIOID AND NONOPIOID ANALGESICS |
||||
|
Tramadol |
50 mg once or twice daily |
Increase by 50-100 mg daily in divided doses every 2
days as tolerated |
400 mg daily; 300 mg daily if patient is >75 years
old |
Drowsiness, dizziness, constipation, nausea, vomiting |
|
ANTICONVULSANTS |
||||
|
Gabapentin |
300 mg at bedtime or 100-300 mg three times daily |
Increase by 100-300 mg three times daily every 2 days
as tolerated |
3600 mg daily |
Drowsiness, dizziness, ataxia, peripheral edema |
|
Pregabalin |
75 mg at bedtime or 75 mg twice daily |
Increase by 75 mg twice daily every 3 days as tolerated |
600 mg daily |
Drowsiness, dizziness, ataxia, peripheral edema |
|
|
||||
|
Nortriptyline |
25 mg at bedtime |
Increase by 25 mg daily every 2-3 days as tolerated |
150 mg daily |
Drowsiness, dry mouth, blurred vision, weight gain,
urinary retention |
|
TOPICAL THERAPY |
||||
|
Lidocaine patch (5%) |
One patch, applied to intact skin only, for up to 12 hr
per day |
None |
One patch for up to 12 hr per day |
Local irritation, if systemic, absorption can cause
drowsiness, dizziness |
Prevention
of postherpetic neuralgia
Very large
randomized placebo-controlled trials of the zoster vaccine in adults older than
60 years revealed a significant reduction in PHN in people who received the
vaccine.
The use of
gabapentin combined with valacyclovir during acute herpes zoster is more
effective in preventing post herpetic neuralgia than treatment with valacyclovir
alone, particularly in patients at highest risk for PHN. So this regimen is
recommended for patients with acute herpes zoster presenting with moderate to
severe pain.
Prevention
of herpes zoster
In later life, immunity against VZV wanes, but can be
boosted by vaccination, that can prevent or reduce the severity of herpes
zoster and its complications, including postherpetic neuralgia. The zoster
vaccine is the same as the varicella vaccine but at a higher virus titer. FDA
approved this live attenuated vaccine (Zostavax®) for
adult ≥50 years of age in 2006. The Advisory Committee on Immunization
Practices (ACIP) recommends a single dose for all immunocompetent individuals’
≥60 years of age, whether or not they have a history of varicella or herpes
zoster. Older adults who have a current episode of herpes zoster may ask to be
vaccinated, but zoster vaccination is not indicated to treat acute herpes
zoster or PHN. The optimal time to immunize an individual after a recent
episode of herpes zoster is unknown, but it is believed that an interval of 3–5
years after the onset of a well-documented case of herpes zoster is reasonable.
A history of
anaphylactic reaction to any of the vaccine components is a contraindication to
the vaccine. The zoster vaccine should not be given
to persons who have severe acute illness, including active untreated
tuberculosis, until the illness has subsided. Persons with leukemia, lymphomas,
or other malignant neoplasm affecting the bone marrow or lymphatic system, or
with AIDS or other clinical manifestations of HIV infection, including those
with CD4+ T-lymphocyte counts ≤200 per mm3 and/or ≤15% of total lymphocytes
should not receive zoster vaccine. Persons on immunosuppressive therapy,
including high-dose corticosteroid therapy, should not receive the vaccine. The
ACIP defines high-dose corticosteroids as 20 mg or more per day of oral prednisone or equivalent for 14
days or more. Low doses of methotrexate (≤0.4 mg/kg/week), azathioprine (≤3.0 mg/kg/day), or
(prednisolone ≤20 mg/day) are not considered to have significant
immunosuppression. The vaccine is also contraindicated in patients receiving
biological therapies but may be given after 3–6 months following discontinuation
of the immune suppression. The use of heat‐treated VZV vaccine,
currently under investigation, may be a safer option in these situations.
When considering the zoster vaccine,
older adults may express concerns about transmission of vaccine virus to other
individuals. Transmission of VZV requires the development of a vesicular rash
containing vaccine virus after vaccination. If there is no rash, there is no
transmission. Zoster vaccine-associated vesicular rashes are very unusual.
Although vesicular lesions may appear at the injection site, vaccine virus nor
wild-type VZV were detected by DNA PCR testing in vesicular fluid. Transmission
of vaccine virus from recipients of zoster vaccine to susceptible household
contacts has not been documented. Thus, immunocompetent older adults in contact
with immunosuppressed patients and susceptible pregnant women and infants
should receive zoster vaccine to reduce the risk that they will develop herpes
zoster and transmit wild-type VZV to their susceptible immunosuppressed contact
and pregnant women and infants. In the unlikely event that an immunocompromised
contact develops a significant illness caused by vaccine virus, he/she may be
treated with standard anti-VZV agents (acyclovir, valacyclovir, or
famciclovir).
FDA Approval
of recombinant zoster vaccine
A recombinant subunit vaccine containing VZV glycoprotein E and the AS01B adjuvant system (HZ/su) administered in two
doses two months apart reduced the likelihood of herpes zoster ~97% and
postherpetic neuralgia ~90% in adults ≥50 years of age. Efficacy of this
vaccine was unaffected by advancing age and persisted for >3 years; severe
injection site reactions and systemic symptoms each occurred in ~10% of
patients.
This
recombinant adjuvant vaccine (Shingrix®) was approved by
the FDA in October 2017 for individuals 50 years of age or older for the
prevention of herpes zoster.